Department of Physical Therapy
Doctor of Physical Therapy Program
Class of 2023
Student Handbook
This is meant to be used as a supplement to the University of Pittsburgh Graduate &
Professional Studies Catalog
(https://catalog.upp.pitt.edu/index.php)
Please familiarize yourself with the contents of both documents.

Table of Contents
Introduction:
Learning SHRS Policies and Procedures 5
About the School of Health and Rehabilitation Sciences (SHRS) 6
University of Pittsburgh Mission Statement 7
Department of Physical Therapy Philosophy, Mission, Vision & Values 8
Non-Discrimination Policy Statement 10
Academic and University Policies:
Academic & Professional Conduct 12
Code of Professional Conduct 13
Academic Integrity Code 16
Roles & Responsibilities of Students 17
DPT Student Dress Code 19
SHRS Social Media Policy 23
DPT Program Academic Regulations
DPT Course Descriptions 25
Quality Improvement & Performance Assessment Project 36
DPT Comprehensive Examination 37
Requirements for Graduation 37
Standardized Grading Scale 38
Faculty Advisors 39
DPT Clinical Education:
Intro to Clinical Education 41
DPT Student Requirements 42
Clinical Education Health Requirements, Clearances, 43
and Certifications/Training
Clinical Education Schedule 44
General Guidelines for Clinical Education 45
Student Use of the Exxat Software Tool 48
Policy on Social Networking 48
Evaluation and Grading 49
Financial Resources:
Tuition 51
Fees 52
Financial Aid & Eligibility for PA Tuition Rates 53
Scholarships and Awards 54
SHRS Information and Student Resources:
Department of Physical Therapy at Bridgeside Point I 58
Forbes Tower 58
SHRS Technology Support Services 59
University Email Accounts 59
SHRS Learning Resource Center 60
Health Sciences Library System 60
Parking/Transportation 61
Disability Resources & Services 62
Student Health Services 62
University Counseling Center 63
Student Health Fees 64
UPMC Health Plan for Students 65
Liability Insurance 66
Student Resources 67
SHRS Contacts 69
Department of Physical Therapy Contacts 70
Student Related Policies & Procedures 76
Main Campus Map 73
Appendix
DPT Technical Standards 76
*After reviewing the material contained in this DPT Student Handbook, please
electronically sign, date, and return the Acknowledgement Form to the
Administrator, Student Services via email.

4
INTRODUCTION
5
Introduction
The Dean, Chair, Faculty, and Staff all join in welcoming you to the School of Health and
Rehabilitation Sciences (SHRS) Department of Physical Therapy (PT) at the University of
Pittsburgh. We are pleased that you have chosen SHRS as the academic environment in which to
pursue your educational goals.
SHRS and Department of Physical Therapy Policies and Procedures
This handbook was developed to inform you of the SHRS and Department of Physical Therapy
policies, procedures, and information that may vary from general University of Pittsburgh
policies. Therefore, we ask that you:
Read the University Catalog thoroughly and familiarize yourself with its contents.
https://catalog.upp.pitt.edu/index.php
Read the Student Code of Conduct thoroughly and familiarize yourself with its
contents.
www.studentaffairs.pitt.edu/wp-content/uploads/2017/10/2017_Code_of_Conduct_Clean.pdf
Read the SHRS Graduate Student Handbook thoroughly and familiarize yourself with
its contents and University/School policies.
http://www.shrs.pitt.edu/current-students/student-handbooks
Read the DPT Handbook thoroughly and familiarize yourself with its contents.

6
About the School of Health and Rehabilitation Science (SHRS)
The mission of the School of Health and Rehabilitation Sciences (SHRS) is to advance the
theoretical base of knowledge underlying the practice of health and rehabilitation disciplines and
professions through research, teaching and professional service.
The SHRS faculty bases their teaching upon research studies, clinical service and participation in
their respective professional associations. Faculty research and service typically occurs through
multi-disciplinary collaboration in diverse health care and research environments. Consequently,
SHRS students are exposed to state-of-the-art curricula, which are continually being reviewed.
Our students are educated and trained to question the basis of current practice, and to challenge
prevailing models and assumptions. The entry-level curricula reflect the importance of effective
team participation in an inter-disciplinary and rapidly changing environment. Emphasis is given
to the student’s development of analytical problem-solving skills and human relations skills
required for effective clinical and supervisory practice. The student is confronted with the
transition between a professional commitment to providing high quality care and service, while
recognizing the effects of competitive pressures and cost constraints upon the health care
organization.

7
University of Pittsburgh Mission Statement
The University of Pittsburgh, founded in 1787, is one of the oldest institutions of higher
education in the United States. As one of the nation’s distinguished comprehensive universities,
the resources of the University constitute an invaluable asset for the intellectual, economic, and
social enrichment of Pennsylvania, while the international prestige of the University enhances
the image of Pennsylvania throughout the world.
The University’s mission is to:
• Provide high-quality undergraduate programs in the arts and sciences and professional
fields, with emphasis upon those of special benefit to the citizens of Pennsylvania;
• Offer superior graduate programs in the arts and sciences and the professions that
respond to the needs of Pennsylvania, as well as to the broader needs of the nation and
the world;
• Engage in research, artistic, and scholarly activities that advance learning through the
extension of the frontiers of knowledge and creative endeavor;
• Cooperate with industrial and governmental institutions to transfer knowledge in science,
technology, and health care;
• Offer continuing education programs adapted to the personal enrichment, professional
upgrading, and career advancement interest and needs of adult Pennsylvanians; and
• Make available to local communities and public agencies the expertise of the University in
ways that are consistent with the primary teaching and research functions and contribute
to social, intellectual, and economic development in the Commonwealth, the nation, and
the world.
The trustees, faculty, staff, students, and administration of the University are dedicated to
accomplishing this mission to which they pledge their individual and collective efforts,
determined that the University shall continue to be counted among the prominent institutions of
higher education throughout the world.
This mission statement was approved by the University’s Board of Trustees on February 16, 1995
and is unchanged to date.
8
Department of Physical Therapy - Philosophy
We believe that physical therapy is an integral part of any health care delivery system whose
goals align with improving the patient’s experience with care (quality, satisfaction) while
improving population health in a cost-accountable fashion.
Our DPT graduates are evidence-based professionals who are: (1) well-grounded in
foundational sciences relevant to the field of physical therapy; (2) focused on the needs of
patients; (3) appreciative of a team-based care approach and (4) accountable to key
stakeholders.
Department of Physical Therapy – Mission, Vision, and Values
The professional physical therapy program at the University of Pittsburgh has a long-standing
tradition of excellence dating back to 1927. We have graduated physical therapists for over
87 years beginning with the DT Watson School of Physiatrics through the program’s transfer
to the School of Health and Rehabilitation Sciences (SHRS) at the University of Pittsburgh.
Throughout the history of the Physical Therapy Program, it has maintained as its mission:
“The advancement of the art and science of physical therapy and rehabilitation
through education, scholarly activity, and professional service.”
Mission Statement
The mission of the Department of Physical Therapy of the School of Health and Rehabilitation
Science is to advance the profession of physical therapy and rehabilitation in general through
education, scholarly activity, and professional service by:
•
Offering a superior entry-level professional physical therapy program that produces a
competent clinician who is able to function as a cost-effective provider, who is a critical
thinker, who embraces the principles of evidence-based practice and is committed to
lifelong learning and professional development;
•
Engaging in research and scholarly activities that advance physical therapy practice
and rehabilitation through the extension of evidence-based practice and
translational research;
•
Offering advanced continuing education and post-professional degree programs
adapted to the physical therapist who is interested in lifelong learning and career
advancement;
•
Making available to local communities and public agencies the expertise of the faculty
in ways that are responsive to the healthcare needs of Pennsylvania, as well as to the
broader needs of the nation and the world and consistent with the primary teaching
and research functions.

9
Vision Statement
Our vision is to graduate DPTs who are prepared to be change agents in transforming
healthcare to achieve the Triple Aim of better care for individuals, better health for populations
and communities, and lowered cost of health care through continuous quality improvement.
Values Statement
While pursuing our Mission and Vision, the Program will act in accordance with its stated
values. Our values are adopted from the APTA Core Values and those of our primary clinical
partner, the University of Pittsburgh Medical Center (UPMC).
Accountability: Active acceptance of responsibility for the diverse roles, obligations, and
actions of the physical therapist including self-regulation and other behaviors that positively
influence patient/client outcomes, the profession and the health needs of society.
Altruism: The primary regard for or devotion to the interest of patients/clients, thus
assuming the fiduciary responsibility of placing the needs of the patient/client ahead of the
physical therapist’s self- interest.
Compassion and Caring: Compassion is the desire to identify with or sense something of
another’s experience; a precursor to caring. Caring is the concern, empathy, and
consideration for the needs and values of others.
Dignity and Respect: We treat all individuals with dignity and respect.
Excellence: Excellence is physical therapy practice that consistently uses current knowledge and
theory while understanding personal limits, integrates judgment and the patient/client
perspective, challenges mediocrity, and works toward development of new knowledge.
Innovation: We think creatively and build excellence into everything we do.
Integrity: Steadfast adherence to high ethical principles or professional standards; truthfulness,
fairness, doing what you say you will do, and “speaking forth” about why you do what you do.
Professional Duty: The commitment to meeting one’s obligations to provide effective physical
therapy services to individual patients/clients, to serve the profession, and influence the health
of society positively.
Quality and Safety: We create a safe environment where quality is our guiding principle.
Social Responsibility: The promotion of a mutual trust between the profession and the larger
public that necessitates responding to societal needs for health and wellness.
10
University of Pittsburgh Notice of Non-Discrimination
http://www.diversity.pitt.edu/about/notice-non-discrimination
The University of Pittsburgh, as an educational institution and as an employer, does not
discriminate on the basis of disability, race, color, religion, national origin, ancestry, medical
condition, genetic information, marital status, familial status, sex, age, sexual orientation, veteran
status or gender identity and expression in its programs and activities.
The University does not tolerate discrimination, harassment, or retaliation on these bases and
takes steps to ensure that students, employees, and third parties are not subject to a hostile
environment in University programs or activities.
The University responds promptly and equitably to allegations of discrimination, harassment, and
retaliation. It promptly conducts investigations and takes appropriate action, including
disciplinary action, against individuals found to have violated its policies, as well as provides
appropriate remedies to complainants and the campus community. The University is committed
to taking prompt action to end a hostile environment if one has been created, prevent its
recurrence, and remedy the effects of any hostile environment on affected members of the
campus community.
For complete details on the University’s Nondiscrimination, Equal Opportunity, and Affirmative
Action Policy (07-01-03) and Sexual Misconduct Policy (06-05-01), please
Visit https://www.diversity.pitt.edu/civil-rights-title-ix-compliance/policies-procedures-and-practices .
11
ACADEMIC AND
UNIVERSITY POLICIES
12
Academic and Professional Conduct Requirements
To successfully complete the DPT program the student must:
(1) Earn a minimum of a “C” or better in every course in the DPT Plan of Study;
(2) Earn a minimum 3.000 grade point average at the time of graduation;
(3) Earn Satisfactory or Honors for all non-graded courses;
(4) Pass all clinical education requirements (refer to DPT Clinical Education section of
this handbook);
(5) Adhere to the Code of Professional Conduct for Physical Therapy students (provided below);
(6) Adhere to the Academic Integrity Code of SHRS and the University; and
(7) Adhere to the University of Pittsburgh Code of Conduct.
Students are permitted to repeat a course in the DPT plan of study only once. Any grade earned in
the repeated course will be recorded on the academic transcript, even if lower than the original
grade. The original course and grade remain on the transcript; however, it is not counted in the
calculation of the program GPA.
With respect to the clinical education courses, a student cannot fail and repeat more than one
clinical education course. Should this situation occur, the student is subject to dismissal from the
program.
Academic Probation
Graduate students who have completed at least 9 credits and whose cumulative GPA falls below
a 3.000 will be placed on academic probation and will receive written notification of this status.
At this point it is the student's responsibility to meet with his or her advisor.
In order to be removed from academic probation, the student will need to achieve a
cumulative GPA of 3.000 within their next two terms of study. Failure to do so may subject
the student to immediate dismissal from the program at the discretion of the Department
Chair.
Students who fail to demonstrate progress toward meeting graduation requirements in a
timely manner may be placed on academic probation or recommended for dismissal from the
program by the Department Chair, in collaboration with the Associate Dean of Graduate
Studies. SHRS reserves the right to terminate a student at any time for academic or other
reasons.
Dismissal from the program is at the discretion of the SHRS Dean, notwithstanding the
foregoing, in the event it is not mathematically possible for a student to remediate their
cumulative program GPA within the next two terms of study, the student may be immediately
dismissed. A student may appeal their dismissal with the University of Pittsburgh Office of the
Provost.

13
SHRS Academic Policy(s) are located on the school website at:
http://www.shrs.pitt.edu/current-students/academic-policies
The Department of Physical Therapy has set forth the following expectations for professional
conduct:
The student is expected to attend all lectures and laboratory sessions (regardless of mode
of delivery) unless otherwise indicated. The student is also expected to actively
participate in classroom discussions and/or activities. Furthermore, the student is
expected to exhibit professional conduct consistent with the following: DPT Student Code
of Professional Conduct; the APTA Guide for Professional Conduct and the Code of Ethics
for the Physical Therapist (located at www.apta.org [“About Us” → “Policies & Bylaws”→
”Ethics”]), and the policy on classroom behavior as listed in each course syllabus.
Code of Professional Conduct
Doctor of Physical Therapy Students
As a student in a professional program you will be expected to understand and demonstrate the
following professional behaviors. These behaviors outline appropriate professional conduct that
is required in both the classroom and in the clinic and are consistent with the APTA’s Core Values
for Professionalism in Physical Therapy.
Accountability: Active acceptance of responsibility for the diverse roles, obligations, and actions
of the physical therapist including self-regulation and other behaviors that positively influence
patient/client outcomes, the profession and the health needs of society.
The student must be able to fulfill commitments and be accountable for his or her actions
and outcomes. The student is responsible for knowing and fulfilling the requirements of
individual courses as outlined by the professor and/or instructor.
The student must be punctual both in the classroom and clinic and make productive and
efficient use of all available learning experiences in the classroom and clinic.
The student adheres to code of ethics, standards of practice, and policies/procedures that
govern conduct in the classroom and/or the clinic.
The student must demonstrate problem-solving skills by the ability to recognize and define
problems, analyze data, develop and implement solutions, and evaluate outcomes.
Altruism: The primary regard for or devotion to the interest of patients/clients, thus assuming
the fiduciary responsibility of placing the needs of the patient/client ahead of the physical
therapist’s self-interest.
The student will place the needs of the patient/client ahead of his/her own in the clinic.
14
Compassion & Caring: Compassion is the desire to identify with or sense something of another’s
experience; a precursor to caring. Caring is the concern, empathy, and consideration for the needs
and values of others.
The student must demonstrate effective interpersonal skills by the ability to interact
effectively with faculty, fellow students, patients, families, colleagues, other healthcare
professionals, and the community.
The student must communicate effectively, both verbally and non-verbally, with others taking
into consideration individual differences in learning styles, language, and cognitive abilities,
etc.
The student must understand the socio-cultural, economic, and psychological influences on
the individual’s life in their environment.
The student must demonstrate teamwork by the ability to perform effectively as part of a
team both in the classroom and clinic by showing respect for others, putting the goals of the
team and/or patient above individual needs, supporting other team members, remaining
flexible and responsive to change, and using proper manners.
Excellence: Excellence is physical therapy practice that consistently uses current knowledge and
theory while understanding personal limits, integrates judgment and the patient/client
perspective, challenges mediocrity, and works toward development of new knowledge.
The student must demonstrate a commitment to learning.
The student must have the ability to self-assess, identify his or her weaknesses, and seek out
learning opportunities through self-direction.
The student must demonstrate critical thinking by the ability to question logically; to identify,
generate, and evaluate elements of logical argument; to recognize and differentiate facts,
illusions, assumptions, and hidden assumptions; and to distinguish the relevant from the
irrelevant.
The student must internalize the importance of using multiple sources of evidence to support
practice and professional decisions.
Integrity: Steadfast adherence to high ethical principles or professional standards; truthfulness,
fairness, doing what you say you will do, and “speaking forth” about why you do what you do.
The student must be honest and trustworthy academically and in the clinic with his or her
patients/clients and colleagues.
The student will abide by the rules, regulations, and laws applicable to the profession.
15
Professional Duty: The commitment to meeting one’s obligations to provide effective physical
therapy services to individual patients/clients, to serve the profession, and to positively influence
the health of society.
The student must represent the profession of Physical Therapy appropriately through ethical
and legal practice, promotion of the profession, respectful behavior, and professional
appearance and demeanor and must adhere to the APTA Core Values that define
Professionalism.
The student must preserve the safety, security, and confidentiality of individuals in all
professional contexts.
Students are encouraged to become members of the APTA and participate, as able in the
Association’s activities at either the local, state, or national level(s).
Social Responsibility: The promotion of a mutual trust between the profession and the larger
public that necessitates responding to societal needs for health and wellness.
Students are encouraged to participate in community or school sponsored volunteerism to
promote health and wellness.
Students should understand current community wide, nationwide, and worldwide issues and
how they impact society’s health and well-being and the delivery of physical therapy.

16
Academic Integrity Code
A student has an obligation to exhibit honesty, and to respect the ethical standards of the
profession in carrying out his or her academic assignments. Without limiting the application of
this principle, a student may be found to violate this obligation if he or she:
1. Refers during an academic evaluation to materials or sources, or employs devices, not authorized by
the faculty member.
2. Provides assistance during an academic evaluation to another person in a manner not authorized by
the faculty member.
3. Receives assistance during an academic evaluation from another person in a manner not
authorized by the faculty member.
4. Engages in unauthorized possession, buying, selling, obtaining, or using of any materials intended
as an instrument of academic evaluation in advance of its administration.
5. Acts as a substitute for another person in any academic evaluation process.
6. Utilizes a substitute in any academic evaluation procedures.
7. Practices any form of deceit in an academic evaluation proceeding.
8. Depends on the aid of others in a manner expressly prohibited by the faculty member, in the
research, preparation, creation, writing, performing, or publication of work to be submitted for
academic credit or evaluation.
9. Provides aid to another person, knowing such aid is expressly prohibited by the faculty member,
in the research, preparation, creation, writing, performing, or publication of work to be submitted
for academic credit or evaluation.
10. Presents as one's own, for academic evaluation, the ideas, representations, or words of another
person or persons without customary and proper acknowledgment of sources.
11. Submits the work of another person in a manner that represents the work to be one's own.
12. Knowingly permits one's work to be submitted by another person without faculty authorization.
13. Attempts to influence or change one's academic evaluation or record for reasons other than
achievement or merit.
14. Indulges, during a class (or examination) session in which one is a student, in conduct that is so
disruptive as to infringe upon the rights of the faculty member or fellow students.
15. Fails to cooperate, if called upon, in the investigation or disposition of any allegation of dishonesty
pertaining to another student, or any other breach of a student's obligation to exhibit honesty.
16. Violates the canons of ethics of the student’s professional discipline.
17
Roles and Responsibilities of the Student
All students are expected to comply with the Rules and Regulations of the University, the
School of Health and Rehabilitation Sciences, and the Department of Physical Therapy.
All students are assigned to a faculty member who will serve as their Faculty Advisor
throughout the DPT program. Regular communication with the Advisor is recommended. If
the student wishes, he or she may request a change in Advisor at any time in the program.
Departmental and course-specific communication is done primarily via e-mail. Students are
expected to check their Pitt e-mail on a regular basis and are responsible for the maintenance
of their Pitt e-mail accounts.
The Department of Physical Therapy requires current information for all students, including:
➢ Name
➢ Address
➢ Telephone number
➢ Emergency contact information
Students must advise the PT department of any changes to their personal information.
The Administrator of Student Services in the Physical Therapy Department will coordinate
course registration each semester. Before each registration period, an email will be sent to
each class listing the core courses to be taken according to the DPT plan of study. The
University of Pittsburgh Registrar’s Office will then block register all DPT students when
semester registration opens. Students are required to check their class schedule in PeopleSoft
to make sure they are registered for all required courses. Additional information regarding
this process can be found on www.shrs.pitt.edu under the student resource section.
Students wishing to take an Independent Study are responsible for completing the
appropriate form(s) prior to registering for the Independent Study. This form must be signed
by the faculty sponsor.
The DPT Plan of Study must be signed and dated.
Students must maintain an updated profile and complete all requirements on Exxat, the
software program used to manage clinical education requirements.

18
All incoming students to the University of Pittsburgh (graduate and undergraduate)
must notify the Student Health Service (SHS) that they meet the immunization
requirements of the University. In order to do this, please go to the SHS website,
review the immunization requirements, then download and complete the “Incoming
Student Immunization Form”.
1. Click on http://www.studentaffairs.pitt.edu/shs/
2. On right hand side, click on “Student Immunization Requirements”
3. Review each topic in the sub menu, then click on “Submission of Immunization Records” 4.
Helpful information:
a. If you do not have the dates of your immunizations, you can have titers drawn and enter
those values
b. It is okay to fill out demographic information and then upload a formal record of your
immunizations with the electronic form if you prefer instead of filling out the dates.
c. The form does not have to be signed by a physician
d. As noted on the SHS site, you DO NOT have to send a formal record in the mail
*Please note that you will need to complete this requirement before classes begin. Once you have
submitted this form to the Student Health Services, please notify the PT Student Services
Administrator, that you completed this requirement. All students should complete this action item by
August 25, 2020.

19
DPT Student Dress Code
I.
POLICY
It is the policy of the University of Pittsburgh’s Department of Physical Therapy that
personal appearance reflects general cleanliness, good grooming and professional
identity. These guidelines were developed in careful consideration of our public image,
infection control and safety. Exceptions to this policy may be made based on verified
medical, religious, and ethnic issues.
II.
PURPOSE
Doctor of Physical Therapy (DPT) students are expected to present a professional,
businesslike image at all times when representing the University of Pittsburgh’s
Department of Physical Therapy. This includes clinical experiences, meetings, labs, classes,
etc. that are held outside of BSP I, and in the classroom when guest lecturers or patients
are present. For patients and visitors, the appearance of the PT staff can be an indication
of the quality of care they can expect. Students are to dress in a manner that encourages
respect for the dignity of staff members, patients, and visitors and enhances the
professional environment of the PT facility. Each facility may have additional dress code
guidelines.
III.
GENERAL GUIDELINES
A professional appearance must always be maintained. Clothing must be clean and neat
and appropriate undergarments must be worn.
The University of Pittsburgh photo ID badge must always be worn during clinical
fieldwork. Some facilities may require facility-specific ID badges.
Failure to adhere to the dress code guidelines will result in corrective action.
A. Guidelines for Students without Uniform Requirements
1. Examples of professional, business attire are:
Men
Women
Suits
Suits
Dress shirts with tie
Dress blouse
Dress slacks
Dress slacks
Sports Coat
Blazer, sweater
Dress shoes
Dress shoes
Dresses, skirts (appropriate length for
business and professional
environment)
20
2. Facilities may prefer students to dress in business casual attire. Students are
expected to present a neat, professional appearance. Examples of appropriate
business casual attire includes:
• Slacks, Trousers or Khakis
• Collared shirts (with or without tie)
• Sports coats or Blazers
• Sweaters or sweater vests
• Skirts
• Long shorts
• Dresses
• Hard-soled, close-toed shoes
3. Colored or decorative sweatshirts, shirts, sweaters, or denim jeans/skirts/shirts
may be worn on special holidays or occasions whenever permission is given from
individual facilities.
B. Guidelines for Students with Direct Patient Care and/or Uniform Requirements
1. Students required to wear uniforms must comply with the facility-specific color
guidelines and dress code.
a. UPMC hospital uniform requirements include:
• Click on “Visit our Cherokee store” on the left side of the page. Students
must wear navy scrub top and khaki scrub pant/skirt
• The Navy/khaki colors must be the same as the Cherokee brand navy/khaki
(different vendors may vary in their shades of navy/khaki)
• Navy scrub coat/jacket may be worn over scrub top
• Only white short or long-sleeve shirt maybe worn under navy scrub top
• Scrub tops/jackets do not need to have UPMC embroidered on the left
chest area
• For convenience, American Discount Uniform is an approved provider for
UPMC and carries scrubs in approved colors/styles. (Students are not
required to purchase Cherokee brand scrubs but should use Cherokee as a
guide to the color-matching).
Website: www.americandiscountuniform.net.
b. If you are at a non-UPMC Hospital, please contact your facility for specific
uniform guidelines.
21
2. In consideration for infection control and patient safety:
• Hair should be neat, clean and pulled back with small simple hair accessories
so hair does not come in contact with the patient. Hair color of an unnatural
tone is not permitted (green, blue, pink, purple, etc.)
• Beards and mustaches should be short, clean, and well-groomed and cannot
inhibit proper respirator fit.
• Maintain good personal hygiene. Offensive body or clothing odor is
unacceptable including odors related to tobacco use or smoking.
• Wearing excessive jewelry is not appropriate. Dangling earrings or hoops
larger than 1/2 inch are not permitted. Earrings are limited to two (2) per
lobe. Facial jewelry, oral jewelry, and gauge earrings are not permitted.
• Makeup should be kept to a minimum. Cologne or perfume is not
recommended as many patients are sensitive to them (includes scented hair
sprays, lotions, etc).
• Nails should be well groomed and not extend more than ¼ inch past the tip of
the finger for patient safety.
• Artificial nails are prohibited; the definition of artificial fingernails includes, but
is not limited to, acrylic nails, all overlays, tips, bondings, extensions, tapes,
inlays, and wraps.
• Footwear must be clean, white, closed-toe duty or leather or vinyl athletic
shoe, primarily white or all black. The athletic shoes must be in good condition
and used for work purposes only. Foot coverings (hose or socks) are required.
3. Colored or decorative sweatshirts, shirts, sweaters, or denim jeans/skirts/shirts
may be worn on special holidays or occasions whenever permission is given from
individual facilities.
C. Displaying Tattoos and Similar Body Art
• Every effort must be made to cover tattoos or body art regardless of size or
placement on one’s body.
22
D. Examples of Inappropriate Attire for Any Student
• Ripped or disheveled clothing
• Stretch knit leggings/yoga pants
• Low cut or low riding pants, excessively baggy pants
• Revealing attire (i.e. midriff tops, tank tops, tube tops, halter tops, tops with
spaghetti straps, very short skirts, shorts blouse with low neckline)
• Clothes which allow your undergarments to be exposed
• T-shirts (only under scrub shirt and must be completely covered by the scrub
shirt)
• Flannel shirts
• Denim shirts or jeans of any type or color
• Hats including baseball caps, inside a building
• Patient gown
• Athletic wear – including silk or nylon warm-up suits
• Spandex outfits
• Clothing displaying slogans or messages
• Casual sandals

23
SHRS Social Media Policy
Social media is rapidly expanding and new outlets are created every day. Professional
organizations and ethical codes are often outdated given the rapid expansion of social media.
It is essential that students and faculty remain aware and vigilant regarding the social media
ethical challenges facing health professionals, clients, patients and students. Students are
responsible for maintaining a professional social media presence related to any SHRS
education activities. Some students may find it helpful to create separate professional and
personal social media accounts.
We recommend that students consider the following prior to posting or transmitting on social
media:
• Consider the audience and potential impact of your post prior to transmission.
• Assume anything that you post or transmit on social media can be viewed by the public.
• An electronic post or transmission is often traceable, without an opportunity for
removal.
• Employers often search social media to learn more about you prior to interviews or
offered employment.
• Clients often search social media to learn more about you. Proximity based apps and
social media post new challenges to maintaining professional boundaries between
health professionals and clients or patients.
SHRS students must:
• Respect the ethical standards of the profession in carrying out their academic
assignments.
• Comply with HIPAA’s social media rules.
• Read, review and follow the social media policy of their practicum or internship
placement.
• Comply with School and University academic integrity guidelines.
• Do not post or transmit any information or reference about their work with clients.
• Do not post clinical encounters, clinical experiences or information that pertains to
working with Clients.
Please note that boundaries on social media are no longer as simple as not ‘friending’ a client,
professor or colleague on Facebook. For example, all contacts in your phone book can read
your posts on Venmo without being friends on the app. It is difficult to predict the next ethical
problem or boundary that will arise with social media. Therefore, please remain aware and
consult with faculty or supervisors on these important issues. Faculty may have to act upon
any material that does not comply with current academic integrity guidelines, professional
ethical standards or HIPAA policies.
On a regular basis review the student bulletin board in the Student Commons area at
Bridgeside Point as updates, announcements, and helpful information may be posted
there.
Check your mailbox and your Pitt email account frequently for important announcements and
information.
If you have any questions, contact the Department of Physical Therapy at 412-383-8169
or the Office of Student Services, 4024 Forbes Tower, 412-383-6551.

24
DPT
ACADEMIC
PROGRAM &
REGULATIONS

25
DPT Course Descriptions
PT 2025– Physiology of Exercise (2 Credits)
In this course, students will learn the structure and function of muscle and principles of
neuromuscular recruitment for physical work. The biophysics of muscle contraction, excitation-
contraction coupling, and contractile biochemistry, including sources of fuel for muscular work,
and shifts in energy demands and fuel sources with physical activity under conditions of steady
state, fasting, exercise and stress will also be covered. Examples of the impact of structural and
physiological changes with growth, aging, disease, drugs, and performance enhancing substances
are reviewed.
PT 2029 – Kinesiology & Introduction to Therapeutic Exercise (3 Credits)
An introduction to the foundations of biomechanics, musculoskeletal tissue mechanics, and
therapeutic exercise that will provide the basic principles underlying the analysis of normal and
pathological human movement with applications to the musculoskeletal system.
This material will be presented in lecture format and will be supplemented by direct laboratory
experience
PT 2030 – Human Anatomy (6 Credits)
Systems and regional approaches to gross human anatomy are combined to study anatomical
components and principles of function. The material covered in this course includes anatomy of
the musculoskeletal, neural and vascular systems of the extremities, head, neck and trunk. Also
included is the anatomy of the heart and lungs. Lectures are complemented by laboratory
experience involving both prosection study of human cadavers and instructional palpation of live
humans.
PT 2026 – Cardiopulmonary PT I (2 credits)
Students learn structure and function of the cardiovascular and pulmonary systems underlying
the delivery of an oxygenated blood to active tissues of the body. Students will gain a basic
understanding of cardiorespiratory fitness and pulmonary physiology in both healthy and
diseased states. Principles of physical training (e.g. conditioning) for persons with and without
cardiopulmonary dysfunction are addressed through lecture, demonstrations, and student
participation in monitoring and interpreting signs and symptoms of physical work in healthy and
disease states. This course will include an overview of the electrical conduction system of the
heart as well as EKG rhythm interpretation. Students will learn contraindication and termination
points for physical therapy interventions during simulated laboratory experiences, case analyses
of cardiovascular and pulmonary assessment data, and skill demonstration.
Prerequisite course(s): PT 2025

26
PT 2031 – Musculoskeletal Physical Therapy I (6 Credits)
This course is the first of the Musculoskeletal series. PT 2031 is an overview of the
musculoskeletal causes and treatments of movement dysfunction related to the lower extremity.
Lecture and laboratory sessions are used to develop competency in the knowledge of
pathomechanics of musculoskeletal injuries, prevention, screening, patient evaluation, treatment
planning and implementation. This course emphasizes the adaptation of this knowledge and skills
into evidence based clinical decision making and assessment of treatment outcome for patients
with lower extremity musculoskeletal dysfunction.
Prerequisite course(s): PT 2025, 2029, 2030
PT 2040 – Survey of Human Disease I (2 Credits)
This course provides an introduction to pathophysiology, epidemiology, and functional
consequences of disease. To develop skills in effective differential diagnosis of musculoskeletal
and non-musculoskeletal conditions, students learn pathophysiologic mechanisms of human
diseases, along with the signs and symptoms characteristic of dysfunction in a given system.
Using an interview-based review of systems, students screen for undiagnosed or uncontrolled
involvement of the immune, hematologic, integumentary, endocrine, and lymphatic systems, and
recognize the need to generate medical referrals or modify a rehabilitation plan of care as
appropriate. Students learn to review medical histories with insight into the potential impact of
comorbid conditions, and the related medical treatments, on the physical therapy examination,
as well as the larger impact on function, activity, and participation. Medical terminology is
introduced for effective interdisciplinary communication. The information in this course serves as
a foundation for clinical management skills covered in Patient Management I and elsewhere in
the DPT curriculum.
Prerequisite course(s): PT 2025, 2029, 2030
PT 2041 – Patient Management 1 (4 Credits)
This course provides an introduction to physical therapy interventions that are used to help
alleviate patients’ movement dysfunction and problems with pain that may be caused by a
variety of pathologies. Developing knowledge and skills in proper patient and therapist body
mechanics, transfer techniques, wheelchair design, patient positioning and draping and use of
ambulatory assistive devices are stressed; as are the knowledge and skills of the physical
modalities of heat, light, cold, water and massage.
Prerequisite course(s): PT 2025, 2029, 2030
PT 2072 – Evidence-Based Practice I (2 Credits)
Introduction to the concepts of evidence-based practice in physical therapy; basic principles of
research in physical therapy interventions, including research methodology, study design,
hypothesis testing, and principles of data collection and outcome assessment; integration of
classroom lecture and discussion, and small-group forums to help students learn how research
evidence impacts the selection of physical therapy interventions; emphasis is on locating and
applying the evidence taking into consideration critical appraisal of the evidence, clinical
expertise and a patient’s unique characteristics, values and circumstances.

27
PT 2089- Clinical Education Seminar (2 credits)
This course will introduce students to the professional behaviors and competencies required to
be successful in physical therapy clinical practice. This seminar occurs in conjunction with the
student’s first clinical education experience and the student is expected to demonstrate these
behaviors and competencies. In addition to a discussion of the expectations for professional
behavior in the clinic, course content includes: therapeutic communication skills, legal issues in a
clinical setting, ethical issues in a clinical setting, principles of learning, patient education skills,
cultural competency principles, self-assessment skills, and patient documentation. Students will
also be introduced to the University of Pittsburgh Clinical Internship Evaluation Tool and learn
how it is used in assessing their performance during the clinical internship. Students will be
introduced to the professional organization, the American Physical Therapy Association, including
its mission, goals, and member benefits. Students will be required to apply and integrate the
concepts to their individual clinical experience throughout the course.
PT 2130 Clinical Education 1 (4 credits)
Students will complete their first full time 4 week clinical education e experience under the
supervision of a physical therapist. The student will be assigned to a facility in acute care,
outpatient orthopedic, inpatient rehab, or Sub-acute care. The primary purpose of this clinical
experience is to allow the development of the student’s professional behaviors in a clinical
setting including but not limited to communication skills, ethical behavior, legal behavior,
cultural competence, self-assessment, and safety issues. In addition, the student will start to
perform those patient management skills that they have learned in the classroom in the first 3
semesters. They will have specific clinical performance benchmarks for their setting to guide
expectations for both the student and the clinical instructor.
PT 2027 - Cardiopulmonary PT II (2 Credits)
In this course students and faculty explore the application of an understanding of the function of
the cardiovascular and pulmonary systems to managing patients with and without
cardiopulmonary dysfunction. Students will understand the impact of disease and injury on the
cardiopulmonary system, the influence of exercise and activity on cardiopulmonary system
performance and design exercise interventions appropriate for the patient’s abilities, define the
dosage of exercise for specific signs and symptoms and treatment objectives, and identify criteria
on which the exercise interventions would be modified. Course content and objectives include
screening and differential diagnosis as it relates to the cardiovascular and pulmonary systems,
examination of the cardiovascular and pulmonary system, as well as the development and
execution of a treatment plan for patients with primary and secondary cardiopulmonary
disorders across the continuum of care.
Prerequisite course(s): PT 2026

28
PT 2032 – Musculoskeletal Physical Therapy II (5 Credits)
This is the second of the Musculoskeletal series. PT 2032 is an overview of the musculoskeletal
causes and treatments of movement dysfunction related to the upper extremity and spine.
Lecture and laboratory sessions are used to develop competency in the knowledge of
pathomechanics of musculoskeletal injuries, prevention, screening, patient evaluation, treatment
planning and implementation. This course emphasizes the adaptation of this knowledge and skills
into evidence based clinical decision making and assessment of treatment outcome for patients
with musculoskeletal dysfunction in the upper extremity and spine.
Prerequisite course(s): PT 2031
PT 2042 – Patient Management II (3 Credits)
This course provides instruction in physical therapy interventions used to help alleviate
movement dysfunction and pain in a variety of patient populations. Content includes: upper and
lower extremity orthotic and prosthetic intervention, pathological processes and physical therapy
management for patients with amputations cancer, wounds, burns, and arthritis, and
intervention for issues in Women’s Health.
Prerequisite course(s): PT 2041
PT 2045 – Survey of Human Disease II (2 Credits)
This course will use the knowledge and resources developed in PT 2040 and 2041 to further the
study of human disease processes. Primary focus remains on the pathophysiologic mechanisms
and clinical manifestations of human diseases, to enable the student to screen for undiagnosed
or uncontrolled involvement of the gastrointestinal, renal/urinary, hepatobiliary, and endocrine
systems, and to subsequently recognize the need to generate medical referrals or modify a
rehabilitation plan of care. Students learn to review medical histories with insight into the
potential impact of comorbid conditions, and the related medical treatments, on the physical
therapy examination, as well as the larger impact on function, activity, and participation.
Students are also introduced to common mental health disorders and a variety of autoimmune
conditions relevant to the field of physical rehabilitation. The information in this course serves as
a foundation for clinical management skills covered in Patient Management II and elsewhere in
the DPT curriculum.
Prerequisite course(s): PT 2040
PT 2060 – Neuroscience (4 Credits)
This course considers the gross and cellular organization of the central nervous system and its
relationship to the peripheral somatic and visceral systems; the physiological properties of
neurons and their associated structures; and the probable mechanisms for the reception,
transmission, and integration of information at spinal, supraspinal, and cortical levels. Concepts
of normal sensory-motor integration, to include the influence of neural centers on motor activity
and postural control, will be considered, and clinical manifestations of dysfunction of major
neural elements will be discussed. The course content and objectives will be accomplished
through varied learning experiences in lectures; guided laboratory sessions and thorough
reflection on the provided course materials is highly recommended to enhance the learning
experience.

29
PT 2131 Clinical Education 2 (4 Credits)
Students will complete their second full time 6 week clinical education e experience under the
supervision of a physical therapist. The student will be assigned to a facility in acute care,
outpatient orthopedic, inpatient rehab, or Sub-acute care. If they were in an outpatient setting
for Clinical Education 1, then they will be in an inpatient setting for Clinical Education 2 and vice
versa. Students will continue to develop both their professional behaviors and their patient
management skills. They will have specific clinical performance benchmarks for their setting to
guide expectations for both the student and the clinical instructor.
.
Prerequisite course(s): PT 2130
PT 2055 – Growth and Development I (2 Credits)
The major emphasis of this course is on the examination, evaluation and treatment of children.
General principles relating to growth and development of the major systems will be reviewed, in
addition to common diseases and diagnoses affecting those systems. The students will learn to
prioritize appropriate examination and intervention strategies for pediatric patients; interpret
results of clinical findings; develop and prioritize problem lists; and formulate treatment goals
that are functional and age appropriate. This course will specifically cover gross motor
development of typically developing children; the musculoskeletal and cardiopulmonary systems.
Students are expected to integrate the basic information covered in Musculoskeletal PT I and II
and Cardiopulmonary PT I.
Prerequisite course(s): PT 2031; 2032; 2060
PT 2061 – Neuromuscular Physical Therapy I (3 Credits)
This is the first of a three-part series of courses which introduce the student to basic neurological
rehabilitation principles. This course is intended to provide the student with the knowledge and
understanding of human movement and function throughout the neuromuscular system.
Students will be introduced to a neuromotor evaluation scheme for patients with neurologic
impairments. Information will be presented regarding motor behavior and motor control as it
relates to normal and abnormal movement and function. Case studies and a problem-solving
format will be used throughout this course.
Prerequisite course(s): PT 2060

30
PT 2073 – Evidence–Based Practice II (2 Credits)
Application of the principles of evidence-based practice to decisions regarding physical
therapy diagnosis and prognosis based on best available evidence; integration of lectures,
discussion, and online resources will assist students as they learn how to appraise the research
literature regarding diagnosis and prognosis, and applying evidence in practice for individual
patients taking into consideration critical appraisal of the evidence, clinical expertise and a
patient’s unique characteristics, values and circumstances.
Prerequisite course(s): PT 2072
PT 2081 PT Leadership & Professional Development I (1 credit)
This course is the first in a series of three (3) that examines the professional practice of physical
therapy. The content focuses on professionalism, code of ethics, regulatory agencies governing
practice, standards of conduct and practice act(s). In addition, it provides an introduction to
documentation, the health care industry, payers, and the continuum of care and how they relate
to the physical therapy profession.
The course series presents management principles for effective and efficient patient care services
by providing knowledge of health care systems, organizational structures and functions, and
personnel management policies in the environments of practice. Standards of practice including
legal, licensure, accreditation, fiscal, ethical, documentation, reimbursement and regulatory, and
information management technologies are considered. Entry level students are prepared for
writing resumes, job interviews, job searches and for continuing their professional development
after graduation.

31
PT 2028 -Health and Wellness (1 credit)
This course examines health and wellness strategies and interventions across the lifespan,
including the role of the physical therapist. It addresses prevention (of illness or injury) initiatives
as well. Participants will be able to identify and assess the health needs of individuals including
screening, prevention, and wellness programs that are appropriate to physical therapy. Students
will be prepared to promote optimal health by providing information on wellness, disease,
impairment, functional limitations, disability, and health risks related to age, gender, culture, and
lifestyle. Concepts of health behavior change, including behavior change theories and
motivational interviewing, are introduced with an emphasis on strategies for promoting
patient/client adherence to a healthier lifestyle. Students are also introduced to nutrition for
optimizing health in normal and diseased states. Learning experiences include lectures,
discussion, case studies, and demonstration.
PT 2033 –Musculoskeletal Physical Therapy III (3 Credits)
This is the final course of the Musculoskeletal series. PT 2033 is an advanced seminar in
evaluative techniques, application and progression of therapeutic intervention. Lecture and
laboratory sessions will consist of advanced seminars by the University of Pittsburgh Faculty.
Specific topics related to task and movement analysis, advance spine and women’s health
concepts, pain and biopsychosocial influence, soft tissue and myofascial techniques. The final
section of this course will be dedicated to ergonomics and its influence on musculoskeletal
injuries. In this section, students will be introduced to human factors in industry, workplace
design, evaluation of work demands, biomechanical analyses of work, work hardening and return
to work principles. Being the culmination of the Musculoskeletal series, competency will be
assessed with written exams, and a comprehensive musculoskeletal oral practical examination.
Upon completion of PT 2033, students will be able to demonstrate knowledge of, and be able to
implement the most current clinical practice guidelines in musculoskeletal physical therapy
practice as it pertains to the Spine, Upper Extremity and Lower Extremity.
Prerequisite course(s): PT 2032
PT 2056 – Growth and Development II (2 Credits)
This course is a continuation of PT 2055 with the major emphasis on the examination, evaluation
and treatment of children with neuromuscular diagnoses and neurodevelopmental delays and
disabilities. Diagnoses commonly seen in Pediatrics will be covered, as well as general
examination and treatment strategies. The students will learn to interpret results of clinical
findings in these patient groups; develop and prioritize problem lists; and formulate treatment
goals that are functional and age appropriate. Students will also learn about specific practice
settings unique to Pediatric practice. The students are expected to integrate the information
presented in the Neuromuscular PT sequences.
Prerequisite course(s): PT 2055

32
PT 2062 – Neuromuscular Physical Therapy II (5 Credits)
This course is a continuation of PT 2061 and is an overview of adult neurological diseases. The
symptoms/prognosis, typical functional limitations, and evaluation/intervention will be
discussed. This course requires synthesis of previous knowledge in order to effectively manage
the client’s movement dysfunction.
Prerequisite course(s): PT 2061
PT 2074 – Evidence-Based Practice III (1 credit)
This course will focus on aspects of evidence-based practice related to quality and process
improvement and its relationship to the process of care and outcomes management. There will
be a focus on translating contemporary approaches to quality improvement into the clinical
environment. Students will be able to develop mechanisms to gauge (1) compliance; (2)
adherence to standards of care and (3) outcome assessment as the basis for clinical performance
assessment. Furthermore, students will apply the FOCUS PDCA (Deming cycle) methodology to
quality and process improvement opportunities in physical therapy practice.
Prerequisite course(s): PT 2073
PT 2082- PT Leadership & Professional Development II (1 credit)
This course is the second in a series of three (3) that examines the environment and conduct of
the professional practice of physical therapy. The primary focus will be upon leadership and
management principles, styles and primary functions essential to practice management. In
addition, we explore professional development and career preparation. Finally, we will explore
effective teamwork dynamics, communication and conflict management strategies and styles.
Learning experiences consist of readings, lectures, and discussions as well as three practical
applications: case study using The Guide, resume and cover letter preparation, and a leadership
development plan.
Prerequisite course(s): PT 2081
PT 2132 Clinical Education 3 (3 Credits)
Students will have the opportunity to explore an area of personal interest in a 12 hour a week
clinical internship. Opportunities may be available in acute care, inpatient and outpatient
neurorehab, homecare, pediatrics, outpatient orthopedics, hand therapy, health & wellness,
wound care, women’s health, and research. The student is expected to continue to develop their
professional skills while acquiring patient management skills specific to each individual clinic.
Prerequisite course(s): PT 2130 and 2131

33
PT 2059 Geriatric Physical Therapy (2 Credits)
The content of the course provides information and sources of information to enable the student
to appreciate changes in physical function (including physical, cognitive and social aspects) of the
older adult and consider the potential impact the changes may have on health status and
assessment and treatment in physical therapy. An overview of systemic, behavioral, and
cognitive changes that typically occur with advanced age and the impact of the changes on
physical function are also discussed. Through lectures, discussions with guest presenters,
systematic review of selected peer-reviewed journal articles, and site visits, students are better
prepared to: 1) recognize signs of depression, 2) understand decisions and discussions revolving
around advanced directives for care, 3) define strategies for communicating and for educating
the older adult, the older adult with dementia, and their caregiver. Skill and experience in using
the peer-reviewed literature in respected journals in the fields of gerontology and geriatrics,
knowledge and identified sources of knowledge about physical performance and assessment of
older adults are used to design an exercise program (and the rationale) for an older adult.
PT 2063 – Neuromuscular Physical Therapy III (3 Credits)
This course is a continuation of PT 2061 and PT 2062. This course combines the theoretical
knowledge of neuromuscular dysfunction previously learned with treatment application. The
causes of dysfunction, assumptions of treatment approaches, and management of patients with
neuromuscular dysfunction are emphasized. This course also covers the assessment and
management of patients with disorders of balance and postural control. The course requires
synthesis of previous knowledge in order to effectively manage the client’s movement
dysfunction.
Prerequisite course(s): PT 2062
PT 2075 Evidence-Based Practice IV (2 Credit)
In this course, an integration of classroom lecture and discussion and small-group research
forums provides students with the knowledge and skills required to collect and analyze clinical
outcomes data for the purposes of assessing clinical performance and developing a personal
performance improvement plan.
Prerequisite course(s): PT 2074
PT 2079- Management of the Medically Complex Patient (1 credit)
This seminar will utilize case studies to examine the management of patient populations with multiple
systems involvement, including illness, injury, impairment, functional deficits, and/or disability.
The focus will be on assessing the student’s ability to screen for medical disease, select appropriate
tests and measurements, evaluate and provide a prognosis, and formulate a plan of care for the
patient. The format of this course will include a case presentation with subsequent discussion in
which students will be able to interact with clinicians and other students for the purpose of
identifying evaluation and treatment strategies for managing the medically complex patient.
Prerequisite course(s): PT 2026;2027;2031;2032;2033;2061;2062;2063

34
PT 2083- PT Leadership & Professional Development III (3 credits)
This course is the third in a series of three (3) that examines the environment and conduct of the
professional practice of physical therapy. We will be exploring the healthcare continuum in which
we as physical therapists practice. We will be examining the rules, regulations, laws, payer
requirements, accrediting agencies’ quality and safety standards, corporate compliance
programs, leadership and management principles, and the “business” of rehabilitation. We will
apply and integrate the concepts learned into real- life group projects and written examinations.
Prerequisite course(s): PT 2082
PT 2102 – Pharmacology (3 Credits)
This is a basic science course covering the principles of drug action for several important classes
of drugs. A course in pathophysiology is a prerequisite for this course and a basic knowledge of
principles of chemistry and biochemistry will be helpful in understanding the chemical basis of
drug-receptor interactions. The course begins with fundamentals of pharmacodynamics and
pharmacokinetics and then covers the pharmacology of the central nervous system, respiratory
system, gastrointestinal system, renal/cardiovascular system, endocrine system, and the
mechanism of action and use of antibiotics
PT 2076 Evidence-Based Practice V (1 Credit)
In this course the student will utilize the database developed in PT 2074 to collect clinical
outcomes and process of care data for all patients managed by the student during a 12 week
period. Students will be required to summarize their compliance with data collection.
Prerequisite course(s): PT 2075
PT 2133 Clinical Education 5 (full-time) (8 Credits)
This will be the first of two semesters of a full-time, terminal clinical education experience
conducted under the supervision of qualified physical therapists in a variety of practice settings.
Students will be assessed using clinical performance benchmarks specific to their area of
practice.
Students are expected to function as an integral part of the healthcare team at their facility. In
addition, students are encouraged to take advantage of supplemental learning opportunities
available at their facility and in the professional community such as participating in
administrative activities, conferences, clinical and academic teaching, or health and wellness
activities, etc. By the end of this experience, students are expected to be able to
independently manage the patient with a familiar diagnosis in their setting as well as display
the appropriate professional behaviors at all times.
Prerequisite course(s): PT 2130-2132

35
PT 2077 Evidence-Based Practice VI (1 credit)
In this course the student will analyze, summarize and interpret the clinical outcomes and
process of care data that were collected in PT 2076 during the 12 week period. Students will
utilize this information to critically evaluate their performance in comparison to their peers
and to develop an individualized performance improvement plan.
Prerequisite course(s): PT 2076
PT 2134 Clinical Education 6 (full-time) (8 Credits)
This will be the second of two semesters of a full-time, terminal clinical education experience
conducted under the supervision of qualified physical therapists in a variety of practice settings.
Students will be assessed using clinical performance benchmarks specific to their area of
practice.
Students are expected to function as an integral part of the healthcare team at their facility. In
addition, students are encouraged to take advantage of supplemental learning opportunities
available at their facility and in the professional community such as participating in
administrative activities, conferences, clinical and academic teaching, or health and wellness
activities, etc. At the end of the experience students are expected to be independent
managing all patients in their setting as well as demonstrating the appropriate professional
behavior at all times.
Prerequisite course(s): PT 2130 to 2133

36
Quality Improvement & Performance Assessment Project
PT 2076-2077: Evidence-Based Practice V-VI
PT 2076 - 2077 are a series of courses in which the student will analyze his/her clinical
performance by collecting and analyzing process of care and clinical outcomes data. Data will be
collected for all patients managed by the student during a 12 week period of his/her final
clinical internship. Students will utilize the database(s) developed in PT 2076 to record process
of care and clinical outcomes data. The student will summarize their compliance with data
collection.
In PT 2076, students will collect outcomes data for 12 weeks, from mid-August to mid-
December on all patients as the standard of care. Patients beginning treatment in December
will be followed until the end of care.
In PT 2077, the data collected in PT 2076 will be analyzed to determine compliance with data
collection, adherence to treatment guidelines and a summary of the outcomes achieved.
Compliance with data collection will be determined as the number of patients with complete
outcomes and process of care data divided by the total number of patients treated. Adherence
to treatment guidelines will be determined as the number of patients receiving the intervention
divided by the number of patients for whom the intervention was indicated. The summary of
clinical outcomes will include a summary of the patients at the start of care, end of care and
change over the course of care in terms of relevant impairments, activity limitations and
participation restrictions.
At the completion of the course, the student will submit a written summary that includes a
description of the patients, compliance with data collection, adherence to treatment guidelines,
summary of outcomes, a comparison of performance relative to other students and a plan to
improve his/her own performance. Particular emphasis will be placed on the student’s critical
analysis of patients that did not attain a clinically meaningful improvement with the intent of
improving future clinical performance. The performance improvement plan should address
what would be done differently when applying this process in the future and a reflection on
how the process of outcomes data collection and analysis contributes to evidence based
practice and the student’s future professional development. Group presentations at the end of
the semester will be done to summarize the data for all students in the class and the results for the
entire process.

37
Comprehensive Examination
Students must successfully pass a written comprehensive examination prior to graduation from
the DPT program. The written examination is given during Term 7. The written examination
consists of multiple-choice questions from four major clinical content areas: Cardiopulmonary,
Patient Management, Musculoskeletal and Neuromuscular.
In order to successfully “Pass” the comprehensive examination, students are required to achieve
≥ 70% on each of the four content areas.
Successful completion of the written comprehensive exam is required for graduation.
Requirements for Graduation
To be eligible to graduate with the Doctor of Physical Therapy degree, the student must:
1. Successfully complete the DPT plan of study;
2. Pass the written comprehensive examination;
3. Successfully complete the Quality Improvement and Performance Assessment Project
during the terminal clinical educational experience;
4. Earn a minimum of a C or better in all graded courses;
5. Earn a Satisfactory or Honors in all non-graded courses;
6. Earn at least a 3.0 grade point average at the time of graduation;
7. Adhere to the Code of Professional Conduct for DPT Students;
8. Adhere to the Academic Integrity Code of the University of Pittsburgh; and
9. Adhere to the Student Code of Conduct at the University of Pittsburgh.
If a student fails to meet any of the above requirements, they will not graduate from the DPT
program.
38
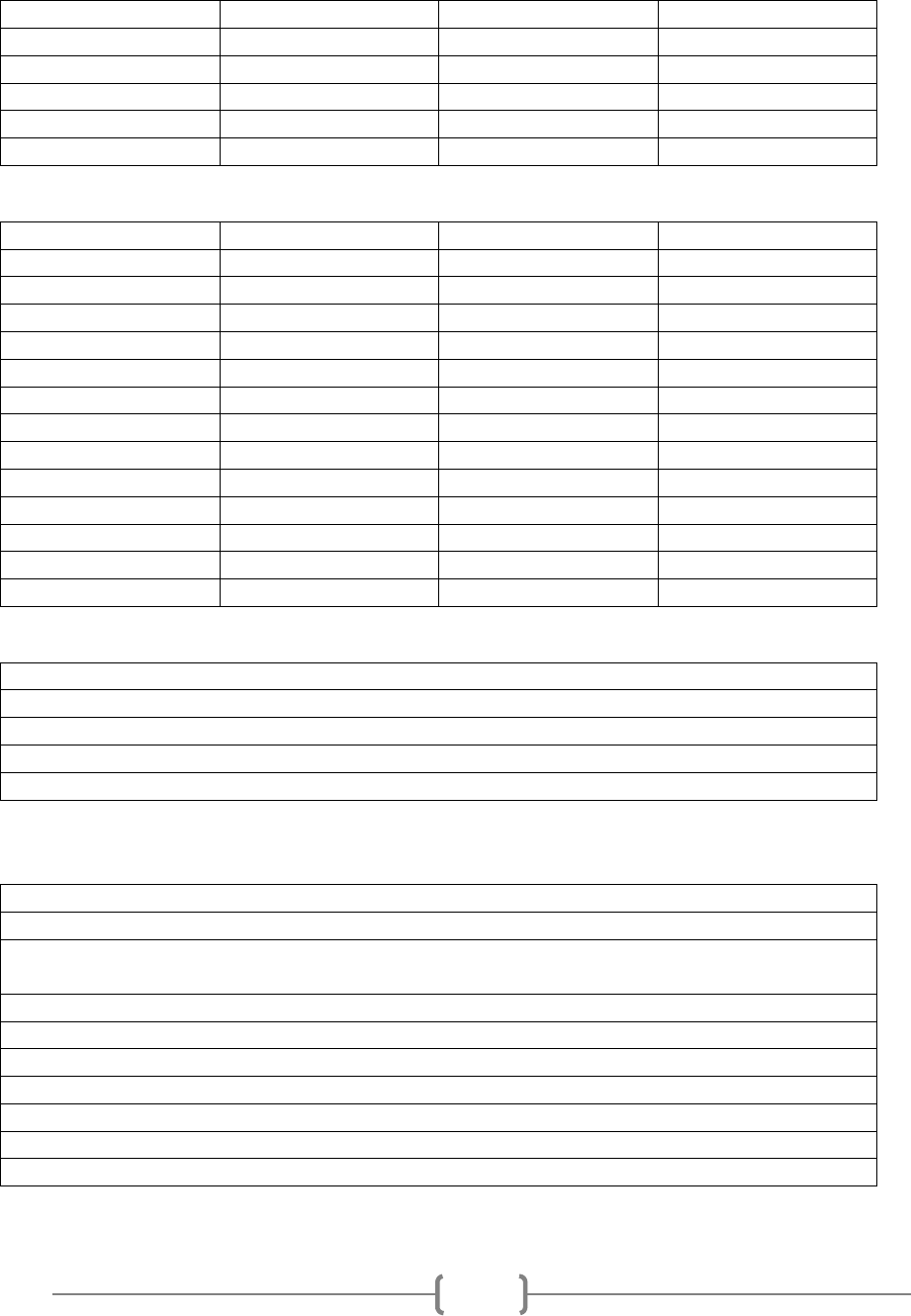
Option A:
Department of Physical Therapy
Standardized Grading Scale
Point Scale
Grade
GPA Value
Graduate
90-100
A
4.00
80-89
B
3.00
70-79
C
2.00
60-69
D
1.00
<60
F
0.00
Option B: Letter Grading System
Point Scale
Grade
GPA
Graduate
99-100
A+
4.00
90-98
A
4.00
Superior
89
A-
3.75
88
B+
3.25
80-87
B
3.00
Adequate
79
B-
2.75
78
C+
2.25
70-77
C
2.00
Minimal
69
C-
1.75
Failure
68
D+
1.25
60-67
D
1.00
59
D-
.75
<59
F
0.00
Option C: Grade Course Options
LG – Letter Grade
H / S / U – Honors / Satisfactory / Unsatisfactory
S / N – Satisfactory / Audit
LG and H / S / U – Letter Grade and Honors / Satisfactory / Unsatisfactory
LG and S / N - Letter Grade and Satisfactory / Audit
* When no grade option is indicated for a course by the department, Letter Grade will be the only option.
Option D: No Quality Points
G – Unfinished Course Work (extenuating personal circumstances)
H – Honors (exceptional) completion of course requirements
I – Incomplete (due to nature of the course, clinical work, or incomplete research work in
individual guidance courses or seminars.
N – Audit (noncredit)
R – Resignation (student resigned from the University for the term)
S – Satisfactory (satisfactory completion of course requirements)
U – Unsatisfactory (unsatisfactory completion of course requirements
W – Withdrawal
Z – Invalid Grade (invalid grade reported)
** - no grade (no grade reported)
39
Faculty Advisors
The Vice Chair, Department of Physical Therapy, assigns faculty advisors for
DPT students. All students will be notified of their Advisor assignment during
DPT Orientation.
If a student prefers to change faculty advisor, she/he should:
➢ discuss it, if appropriate, with current advisor;
➢ contact the Vice Chair’s office
Advisor’s Roles and Responsibilities
The advisor’s role is to help guide the student’s progress through the DPT program.
The Faculty advisor will:
Meet with the student after the start of the curriculum;
Assist the student in the following: choosing and registering for electives, engaging in student
leadership roles, participating in extracurricular/service activities
Meet with the student periodically throughout the program;
Be available to the student on a regular basis;
Meet with the student as needed to review academic progress; and discuss professional plans;
Meet with the student upon his/her notification of probationary status;
Assist the student with accessing academic/student-related/professional resources as needed.

40
DPT CLINICAL EDUCATION

41
Introduction to Clinical Education
Our clinical education curriculum consists of a combination of experiences integrated
throughout the curriculum as well as a terminal experience at the end of the didactic
curriculum. Students will complete a 4-week full time clinical education experience in their
first summer, a 6-week full time clinical education experience in their 2nd spring, and a part
time clinical education experience in their second summer as integrated experiences. At
the end of the didactic curriculum they will complete a 30-week terminal clinical education
experience which can be one rotation or two 15-week rotations. In total our DPT students
will complete 40 weeks of full-time clinical education experiences.
Our clinical education experiences occur primarily within the University of Pittsburgh
Medical Center (UPMC), an integrated health system and its affiliates. In addition, we have
established partnerships with select clinical facilities within the Greater Pittsburgh area.
This allows us to provide clinical experiences are across the continuum of care in a variety
of settings including acute care hospitals, skilled nursing facilities, inpatient acute
rehabilitation facilities, home health agencies, outpatient facilities, and specialty facilities
such as pediatrics, sports medicine, women’s health, balance and vestibular, occupational
health, and hand therapy as well as across the lifespan. While the majority of our clinical
education is in the Greater Pittsburgh area, we have vetted some sites outside the area to
provide opportunities in unusual settings as well as accommodate student’s special needs.
In addition, UPMC has sites throughout western and central Pennsylvania. Students may
be asked to relocate for a full-time clinical education experience in order to provide an
optimal experience for all students.
The academic and clinical faculty share responsibility for defining, implementing, and
evaluating our clinical education program as it is a continually evolving system that is
responsive to the needs of society, the health care system, the physical therapy profession,
and the academic institution.
42
University of Pittsburgh Department of Physical Therapy Clinical Education Requirements
You will begin the clinical education portion of the DPT curriculum in your first summer term (Term 3) and as
such, you are required to meet specific requirements mandated by the clinical sites and the University of
Pittsburgh. These include health requirements, background clearances, and specific training modules. All
requirements must be completed prior to starting Clinical Education 1 in the first summer semester. Please
review the following list of requirements. Please note that if you do not have a clean background check or a
clean drug screen you may not be able to participate in Clinical Education and therefore will not meet the DPT
requirements for graduation. Additionally, many states will inquire whether the applicant has been convicted of
a misdemeanor, felony, or a felonious or illegal act; if you have a record you may not be able to obtain a PT
license to practice your profession after graduation.
You will be uploading these requirements to your Exxat dashboard where they will be approved, reminders of
due dates and expirations will be noted, and they will be sent to your clinical sites where you are placed. There
will be an orientation early in the program to the Exxat system.
*Please note that you may be asked to provide hard copies of required forms so you should always have a hard
copy available to you (preferably the original).
**If you have any physical restrictions in the clinic, fail the drug test, or have a criminal history listed on your
clearances it is your responsibility to meet with the Vice Chair of Clinical Education immediately to discuss the
implications for clinical participation and licensing upon graduation.
Health Requirements
1. Physical examination:
Within a year of the start date of each clinical a physician must sign off that you are physically able to
participate in a clinical education experience.
a. In year one a physical exam should be completed between January 1 and May 15, 2021 using the
Health Appraisal Form provided on Exxat
Note that you must complete all requirements listed on the health form without exception.
b. In year two, a second physical exam must be completed between January 1 and March 15, 2022
using the Health Appraisal Form.
2. TB Test:
a. In year one, the first PPD test should be a 2-step coordinated with your physical exam
b. In each year thereafter you can do the 1-step PPD test; however, please be aware that some
clinics require a 2-step each year. The student is responsible for asking their clinical site if
they require a 1-step or 2-step.
*The TB test is valid for one year and must be repeated before the previous test expires.
43
3. Drug Screen:
Within a year of the start date of each clinical you must have a negative drug screen. The drug test will screen for
marijuana, cocaine, amphetamines, opiates, and PCP. Information for obtaining the drug test is on Exxat. Some
clinical sites require the student to have a drug test immediately prior to the start of the clinical; it is the student’s
responsibility to check with the individual clinical site.
a. In year one, the drug test should be performed between May 4 and June 15, 2021
b. In year two, the drug test should be performed between January 1 and May 31, 2022
Background Clearances
Students are required to obtain background checks prior to the start of their first clinical. Information will be
provided in the first fall semester about obtaining your clearances. Clearances obtained prior to the first fall
semester will not be considered current. Each clinical site also retains the right to request that any of the
clearances be more current than that required by the University. Clearances include:
i. Pennsylvania Act 33 Child Abuse History
ii. Pennsylvania Act 34 Criminal Background Check
iii. Act 73 Clearance FBI History
Miscellaneous Requirements
a. CPR Certification ONLY through the American Heart Association including AED training. This must always
be current. No other training will be accepted.
b. Health Information Portability and Accountability Act (HIPAA) training through the School of Health and
Rehabilitation Sciences (SHRS) must be completed in the first fall semester and remains valid for 3 years
from the date of training. Information about completing the training will be available on Exxat
c. Blood Borne Pathogen training through SHRS must be completed in the first fall semester and repeated
annually. Information about completing the training is available under “Required Documents”.
d. Student must maintain personal health care insurance throughout the duration of the program.
e. Professional Medical Liability coverage is provided through the University of Pittsburgh and the cost
associated will be reflected on your tuition bill.
July 2020
44
Clinical Education Schedule
DPT Year 1
Clinical Education 1
Full time 4 weeks summer term
(Term 3)
DPT Year 2
Clinical Education 2
Full-time, 6 weeks, Spring term
(Term 5)
Clinical Education 3
Part-time, 12 hours a week, Summer Term
(Term 6)
DPT Year 3
Clinical Education 4-& 5 30-week Terminal Clinical Education Experience (Terms 7 & 8)

45
General Guidelines for Clinical Education
Assignment of Students
1.
The Vice Chair of Clinical Education along with the Clinical Education Coordinator
(CEC) in the Department of Physical Therapy will assign students to clinical sites
based on individual need, clinic availability, and academic requirements. Students will
have an opportunity to review available sites and list preferences prior to the
assignments using the Exxat Placement System (see ‘Student Use of Exxat’). Although
the CEC will consider the student’s preferences, there is no guarantee based on the
above factors.
2.
All students are assigned to at least one outpatient and one inpatient site for Clinical
Education 1 and Clinical Education 2
3.
Students will have the opportunity to explore any area of physical therapy for Clinical
Education 3 based on availability
4.
For the students terminal clinical education experience, they may choose to do one
30 week rotation or two 15 week rotations in the following settings, Outpatient
orthopedics, Outpatient Neurologic, Outpatient Women’s Health, Inpatient acute,
Inpatient Rehab, Sub-Acute Rehab, or Pediatrics Inpatient/Outpatient. Assignments
will be made considering the student’s preferences and availability of the sites by the
Vice Chair and the CEC in coordination with our partners.
5.
Although every attempt will be made to place a student in the Greater Pittsburgh
area, we do use placements outside the area that are within the UPMC System and a
student may be required to relocate for a full-time experience.
6. Student assignments will be sent to the sites’ Facility Directors and/or the Site Coordinator of Clinical
Education (SCCE) using the Exxat system. The student will be responsible for keeping an updated
profile on the Exxat System to be shared with the site.
Clinical Education Requirements
1. All students are required to complete one part-time (12 hours a week for a semester),
two full-time (four & six weeks), and a 30 week terminal clinical education experience
to fulfill the DPT plan of study.
2. Students are responsible for contacting the clinical instructors at least one month prior to
the start of their clinical education experiences to arrange their schedules and to confirm
that they have met all site prerequisites.
3. Students are responsible for setting up their Exxat account to manage their clinical
education program and they are responsible for completing all clinical requirements
prior to the start of their first clinical education experience.
*The student is responsible for the costs related to completing clinical requirements.
46
4. Students are expected to maintain and update their Exxat dashboard and
complete all requirements using the Exxat system throughout the three years of the
DPT program. This information will be shared with the clinical sites as needed.
5. Prior to beginning any of the clinical education experiences, students are required to
meet and verify the health requirements of each clinical site to which they are assigned.
At minimum, students are required to complete a physical examination, a drug test, and
TB test within a year of the start of each clinical.
Upon request by the clinic, a student may need to present a hard copy of any of the
required documents.
*Please note that students who are not immunized will not be able to participate in clinical education
6. Students are responsible for obtaining & maintaining private health insurance
throughout the DPT program. The Student Services Health fee assessed each term is
not a substitute for private health insurance.
7. Students are responsible for transportation to and from their clinical sites, and all costs
incurred for transportation, which may include cost and maintenance of an automobile,
public transportation, gas, and parking. Every effort is made to identify clinical site
locations within an approximate 60-mile radius from the University although a few of the
full-time clinical sites are more than 60 miles from the University’s campus.
8. Students may be responsible for locating and paying for housing if a full time site is
outside of the Pittsburgh area.
9. Clinical sites commit to a student’s clinical education experience for the University of
Pittsburgh up to a year in advance, thus changes to a student’s clinical placement are
not made for personal reasons or student preference. However, it is the prerogative of
the faculty to change a student’s clinical placement based on the academic needs of the
student or the request of the clinical site.
10. The student should contact the Vice Chair of Clinical Education, the Clinical Education
Coordinator or other academic faculty with any questions or concerns prior to or during
the clinical education experience. At the University of Pittsburgh, our policy is to address
issues as early as possible, rather than allowing them to persist. Please refer to the
Clinical Education Team Summary resource for contact information. (see Appendices)
11. Site visits from the Vice Chair, the CEC or other faculty can be requested at any time.
12. Students with disabilities must make the request for accommodations prior to the start of
the clinical education experience. We will contact the clinical coordinator at the site to
make the necessary arrangements.
Attendance
1. Clinic attendance is mandatory. In the event of an unavoidable absence or illness, the

47
student should contact both the Vice Chair or CEC and the clinical instructor (CI).
2. Students should attempt to make up any absences during the following week if possible.
3. If frequent absence becomes a concern, the Academic Program, the CI, and the
student will address the issue.
4. During the part-time clinical education experience, students will follow the same
schedule each week, as the CI cannot accommodate changing schedules. Please plan
accordingly for academic deadlines/exams.
5. On occasion, clinic time may be pre-empted by a special presentation or guest
lecture arranged by the Department of Physical Therapy. It is the responsibility of the
student to inform the CI if this occurs.
Dress Code
The student is expected to adhere to the dress code policy at their respective clinical sites. Students
should also note the Department of Physical Therapy Dress Code as outlined in this DPT Student
Handbook.
Policy on Social Networking
The University of Pittsburgh’s Department of Physical Therapy has adopted, and requires the
students to abide by, the UPMC Social Networking policy during all clinical education
experiences. At no time should a student be posting pictures, information, or any type of
comment about a patient or clinical site on any type of social media. Please review the
following UPMC social network policy:
https://www.upmc.com/patients-visitors/privacy-info/social-media-post-policy

48
Student Use of the Exxat Clinical Education Software Tool
The University of Pittsburgh Department of Physical Therapy uses an online software tool, Exxat, to
manage our clinical education program. This system is used for clinical education data, clinical site
data, making placements, communications with students and sites, and managing clinical
evaluation tools. All DPT students should have an active account on the Exxat portal.
The following is a summary of DPT student use of the system as part of clinical education:
1. Students will maintain a dashboard on Exxat, which provides a profile to their clinical
sites including demographic information, contact information, and a history of their
clinical experiences.
2. Students will upload required documents to their dashboard for approval and viewing
by their clinical sites. Please see “Clinical Education Required Documentation” for
details. Hard copies of any documents must be provided to the clinic upon request.
3. Students will complete a clinical questionnaire for each placement to give the site
advanced information about their goals for the placement.
4. Students can get information about the clinical sites we use and read past
student evaluations of their experiences at those sites.
5. Students will have access to the clinical education curriculum and resources on Exxat.
6. Students will complete a “wish list” for each clinical education assignment which will
be considered in the placement process, although there is no guarantee that the
clinics on the wish list will be available or meet the student’s needs.
7. For each placement, students will have a “To Do” list on Exxat with required
activities. Some activities will be completed electronically on the Exxat website while
other activities will be completed separately and uploaded to Exxat.
At minimum for each clinical education experience the student will:
a. Provide contact information and demographics about their clinical instructor (CI)
b. Complete a clinical site orientation
c. Complete a performance improvement plan
d. Complete a midterm and final self-assessment of their clinical performance
e. Complete a midterm and final evaluation of their clinical instructor
f. Complete a final evaluation of the clinical site
8. For each clinical placement, the student’s clinical instructor will complete a midterm and final
evaluation of the student’s clinical performance using an electronic tool, the University of Pittsburgh
Clinical Internship Evaluation Tool (see below).,

49
Evaluation & Grading
1. The electronic version of the University of Pittsburgh Clinical Internship Evaluation Tool
(CIET) will be used by the clinical instructor in the evaluation of students at the midpoint
and conclusion of the clinical education experience. Students will also complete the
electronic CIET as a self- assessment and submit it to their CI who will then complete
their part of the CIET. Students are expected to review both evaluations with their CI and
then submit electronically using Exxat.
2. Students will evaluate their clinical education experience using the electronic PTSE 1
(Student Evaluation of the Site) form on the Exxat site. This should be done at the
end of each clinical education experience.
3. Students will provide feedback to their CI at both the midterm and final points during
each clinical education experience using the electronic PTSE 2 (Student Evaluation of
their CI) form on the Exxat site.
4. At all times, students are expected to comply with the Code of Professional Conduct
for Physical Therapy Students. (Refer to the Code of Conduct included in this DPT
Handbook). Non-compliance may result in failure of the clinical education experience
and possible dismissal from the DPT program.
5. Please review the specific objectives and clinical performance benchmarks for each
clinical education experience as performance on these will provide the basis for
grading.
6. The determination of the grade received (H/S/U) for all clinical education experiences
is a joint decision between the CI and the academic faculty. If a student receives a ‘U’
grade they will be expected to repeat the clinical education course which may result
in an extended plan of study in the DPT program. As noted previously, a student
cannot fail more than 1 clinical education experience. In the event this situation
occurs, the student is subject to dismissal from the program.
7. The clinical placement site may request termination of the clinical experience at any
time if the student is not complying with the Code of Professional Conduct, and/or not
making significant progress in their performance, and/or the student’s health does not
warrant continuation, and/or the student’s conduct or health is a detriment to the
functioning of the clinic. This may result in failure of the clinical education course.

50
FINANCIAL RESOURCES
51
Tuition
Making Payments
There are several options for making tuition payments. You may pay online through PittPAY by e-
Check (free) or credit card (service fee applies). You may also mail check and money order
payments along with the remittance form. Payments can be made in person at the Student
Payment Center, but keep in mind that they do not accept credit card payments in person.
Pre-Pay
This free form plan permits you to reduce your student account balance prior to receiving the
first e-Bill for a new term. You may send any amount you wish and make as many payments as
you wish provided they are received by the date established on the prepayment plan form.
Pay Online (PittPAY)
Payments made by e-Check are offered at no charge. While the University does not accept credit
card payments directly, they have arranged for a third-party vendor to accept American Express,
Discover Card and MasterCard when payment is made online through PittPAY. You will be
charged a non-refundable service fee of 2.75% by the vendor for this service.
Payment can be made by e-Check (electronic check) from an existing checking account, or by
Discover, MasterCard, or American Express.
Students can also authorize parents, guardians or other third-party payers to view their e-Bills
and make payments online.
Students assign the login ID and password and provide it to the authorized individual(s).
Students access the account at https://my.pitt.edu. Once logged in, students can select
PittPAY on the right side of the screen.
Authorized Payers log in at http://payments.pitt.edu/ using the Login name and Password
provided by their student.
Students and Authorized Payers can view and print a copy of the monthly e-Bill.
Students and Authorized Payers can establish payment profiles for their convenience.
Students will receive an e-mail at their official University of Pittsburgh e-mail account when
eBills are available in Pitt PAY
Authorized Payers will be notified at the e-mail address they provide in PittPAY.
Students and Authorized Payers may elect to receive email confirmations of online payments
made by the individual.
Existing Discover/MasterCard/AMEX regulations prohibit the University from making a refund to
you in cash or by check when you made your payment by credit card and there is an adjustment
made to the charges paid. When you pay by credit card and there is a reduction in the amount of
the charges, we are required to credit the credit card account you used to make the payment.
The vendor will not refund any portion of the service fee when you are refunded.

52
Access and payment of your tuition bill
• To access your e-Bill:
Student: log in to https://my.pitt.edu :
• Click on -> PittPAY on the right-hand side of screen
• Click on -> Account Activity on the top tab
• Under appropriate term, click on -> see details
• To pay your e-bill:
Student: log in to https://my.pitt.edu :
• Click on -> PittPAY on the right-hand side of screen
• Click on -> Account summary or Account Activity on the top tabs
• Select Make Payment
Payment must be received by the due date to avoid the assessment of a Late Payment Fee.
Drop Off
You may make your payment in person at G-9 Thackeray Hall or you may drop your payment in
the depository located outside the Student Payment Center on the Ground Floor of Thackeray
Hall. Please do not include cash when using the depository.
If you have any further questions, you may contact the Student Payment Center via phone
Fees
Course Fees
Some courses have fees associated with enrollment in the course. These courses are identified in
the Schedule of Classes and Course Descriptions. The Schedule of Classes is online at:
http://www.registrar.pitt.edu/courseclass.html
Mandatory Fees
The following are mandatory fees assessed to students each term. Current rates are available
online at https://ir.pitt.edu/graduate-tuition/
• Computing and Network Service Fee
• Student Health Fee
• Activity Fee
• Security, Safety, and Transportation Fee
53
Financial Aid
https://financialaid
.pitt.edu/
412-624-7488
The Financial Aid Information Page www.finaid.org
Collegenet www.collegenet.com
College Board on line www.collegeboard.org
Internet largest free scholarship search www.fastweb.com
Eligibility for Pennsylvania Tuition Rates:
http://payments.pitt.edu/pa-tuition-rate-eligibility/
(412-624-7610)
Tuition rates for the University of Pittsburgh are based on whether the student is a
permanent resident of the Commonwealth of Pennsylvania. A higher tuition rate is charged to
nonresidents.
A student who has lived in the Commonwealth of Pennsylvania for 12 consecutive months
immediately prior to enrollment at any college or university in the state may be eligible for
reduced tuition rates. To qualify, the student must also be a citizen of the United States or have
a U.S. immigrant/permanent resident visa. Students under 21 years of age are presumed to have
the same domicile as their parents.
Copies of detailed “University of Pittsburgh Tuition Eligibility Guidelines” are available upon
request in the Students Appeals Office, located in Thackeray Hall.
Any admitted student who does not automatically qualify may petition for reduced tuition rates
and supply additional information to be reviewed by the Student Appeals Coordinator. To be
effective for a particular term, petitions must be submitted within the first 30 calendar days of
the term or 15 calendar days of the session.
Due dates will not be extended, and late payment or late registration fees will not be waived for
any reasons related to the determination of eligibility for reduced tuition.
A student who changes his or her domicile from Pennsylvania to another state must promptly
give written notice to the University. In addition, a student under 21 years of age must report a
change in his or her parents’ or legal guardians’ address.

54
Scholarships & Awards in the Department of Physical Therapy
Scholarship applications (Departmental or SHRS/University) are generally distributed at the
beginning of the fall term each year.
Mary Behling Browne Physical Therapy Scholarship
Established in 2013, this award is used for tuition support of eligible students in the Department
of Physical Therapy at the School of Health and Rehabilitation Sciences at the University of
Pittsburgh. Awards may be made to Physical Therapy students who are in their second or third
year of study with demonstrated financial need.
Dorothy Bradley Brown Endowed Student Scholarship
Established in 1990 by Dorothy Bradley Brown, a 1941 graduate of D.T Watson; this scholarship is
awarded to a DPT student who is enrolled full time, is in good academic standing, and has
financial need. This scholarship can be awarded to one or more students.
Dorothy Bradley Brown Nationality Room Scholarship
This scholarship is awarded to a DPT student in good academic standing who wishes to study
abroad. The scholarship is awarded by the Nationality Rooms scholarship committee.
The purpose of the international study is to:
• Gain exposure to healthcare system(s) outside the United States of America;
• Observe physical therapy practice in other countries
Students interested in exploring the Dorothy Bradley Brown Scholarship should notify the Chair
of the PT Department & the Director of Clinical Education so that planning and coordination of
this experience can be done efficiently. The student may be asked to present at PT Clinical
Rounds after completing the independent study abroad.
Pat Croce Endowed Student Scholarship
Established in 1991 by Pasquale “Pat” Croce, a 1977 graduate of the University of Pittsburgh’s
Department of Physical Therapy; this scholarship is awarded to full time DPT student in the first
year of study who has completed a minimum of 20 credits of professional study in good academic
standing and has financial need. It may be awarded to one or more students.
Centers for Rehab Services (CRS) Leadership Scholarship
Established by Centers for Rehab Services, a partner of UPMC; this scholarship is awarded to an
entry-level physical therapy student(s) demonstrating leadership by way of involvement with
APTA, the Foundation for Physical Therapy, or other roles within the profession. This award is
made at the discretion of the Chairman of the Department of Physical Therapy.

55
Mary K. Daly-Crum Student Award in Physical Therapy
Established in 2012, this award is used to provide support for books, lab fees, travel or other
educational expenses to students in the Department of Physical Therapy at the School of Health and
Rehabilitation Sciences. Preference shall be given to out-of-state students with need.
David Physical Therapy and Sports Medicine Scholarship
Established in 2005 by Joseph David, a 1988 graduate of the University of Pittsburgh’s
Department of Physical Therapy; this scholarship is awarded to an entry-level physical therapy
student in the final year of study who demonstrates financial need; good academic standing
(minimum of 3.0); and exceptional clinical competence. An application, essay, and possible
interview are required.
Victoria Green Scholarship
This scholarship is awarded to physical therapy students in good academic standing.
Patricia Leahy Memorial Scholarship
Established in 1997 in memory of Patti Leahy, a 1979 graduate of the University of Pittsburgh’s
Department of Physical Therapy; this scholarship is awarded to a well-rounded DPT student who
has a special interest in neurology and neurologic physical therapy. The recipient should also
reflect Patti’s love of family, friends, and social life.
Pearl C. Mann Scholarship Fund in Physical Therapy
Established in 1997 by Pearl C. Mann, a 1945 graduate of D.T. Watson; this scholarship is
awarded based on outstanding academic achievement and financial need. The student must be
enrolled full-time in the DPT program and they must be a U.S citizen.
Alice Chagnot Oulette Endowed Student Scholarship
Established in 1991 by Alice Chagnot Oulette, a 1947 D. T. Watson graduate; this scholarship is
awarded to a DPT student who is enrolled full time, is in good academic standing, and has
financial need. This scholarship can be awarded to one or more students.
Paul and Judy Rockar Endowed Student Scholarship
Established in 2005 by Paul (and Judy) Rockar, a 1981 graduate of the University of Pittsburgh’s
Advanced Master’s Orthopaedic and Sports physical therapy program; this scholarship is
awarded to a 2
nd
year DPT student who is enrolled full time and who is in good academic
standing. This student must demonstrate a commitment to professional development,
leadership, and lifelong learning.

56
PT Leadership Development Award
The Physical Therapy Leadership Development Gift was established in 2013 by Debora L. Miller,
1978 graduate of the Physical Therapy program, in honor of her mother, Dorothy Tear Lewis. The
purpose of the annual gift is to offset the expenses associated with the DPT student awardee(s)
participation in the LAMP Institute for Leadership in Physical Therapy of the Health Policy and
Administration Section of the American Physical Therapy Association.
D.T. Watson Alumni Scholarship
Established by the alumni and friends of the D.T. Watson School of Physiatrists, Division of
Physical Therapy, in 1969; this scholarship is awarded to a DPT student who is enrolled full time,
is in good academic standing, and has financial need. This scholarship can be awarded to more
than one student.
Jessie Wright Scholarship
This is the highest honor awarded by the Faculty in the Department of Physical Therapy and is
given to a student who displays superior achievement & potential of becoming an outstanding
clinician. This award is based on the unanimous decision of the Faculty.
Additionally, students will receive notification from the SHRS Student Services representative
related to school-wide scholarship opportunities. Notification of the specific scholarship
options and due dates are shared with students during the Fall semester.

57
SHRS INFORMATION &
STUDENT RESOURCES
58
Department of Physical Therapy at Bridgeside Point I
The Department of Physical Therapy and the Doctor of Physical Therapy (DPT) program are
located at Bridgeside Point I (BSP), along Technology Drive in south Oakland. The building is
secure and requires a registered access badge to gain entrance to all spaces. The building is
accessible 24 hours a day, 7 days a week, and has a security guard in the main lobby from 7 a.m.
to 7 p.m., Monday-Friday.
The PT program has more than 8,000 square feet of instructional space that includes two
classrooms, three clinical labs, and storage space. The Student Commons area is comprised of
two quiet study areas, a lounge with flexible seating and an equipped kitchenette. The Student
Business Center has six PCs, 1 printer, 1 copier, 1 scanner and a centralized mail area.
The Anatomy Lab is located on the 3
rd
floor of BSP 1. DPT students will be in the Anatomy lab
during the first term (Term 1) for the Anatomy lab portion of the course; they will also use the
lab during the Neuroscience labs, which takes place during Term 3.
Mailboxes are assigned to all students in the DPT program, and are located on the 1
st
floor of
BSP. Please note that it is the student’s responsibility to check his/her mailbox regularly as
they may be used for official Pitt, SHRS, Departmental, or personal correspondence.
All student areas on the 1
st
floor of BSP I exit directly to a patio equipped with outdoor seating.
There is also immediate access to walking and biking trails along the Monongahela River.
Parking is available in the Technology Center Garage, operated by the City of Pittsburgh, across
from Bridgeside Point II.
Forbes Tower (SHRS Student Services)
The School of Health & Rehabilitation Sciences (SHRS) is in Forbes Tower, located on Atwood
Street, off Forbes Ave. All SHRS Student Services are located on the 4
th
floor of Forbes Tower.
The front doors to Forbes Tower are open Monday-Thursday between 6:30 a.m.-8:30 p.m.;
Friday, 6 a.m. – 6 p.m.; Saturday, 8 a.m.-5 p.m.; Sunday, (Pitt ID badge required).
Students are encouraged to use the stairwells on the southeast side of the building between the
4
th
and 6
th
floors. However, stairwells cannot be used to enter or exit the building. Students
must use elevators to access the 1
st
floor (entrance/lobby).
The Forbes Tower elevators (including garage levels) are open Monday – Thursday between
6:30 a.m. and 9:30 p.m.; Friday, 6:30 a.m.-6 p.m.; Saturday, 8 a.m.-5 p.m. Access to the
building on Sunday requires prior notice
59
Technology Support Services
6048 Forbes Tower
All Pitt students may use the computers and software available at the public University
computing labs free of charge. For other University computer lab locations, software available
through CSSD and other University technology information, visit:
http://www.technology.pitt.edu/.
More information on SHRS and University technology resources can be found at:
http://www.shrs.pitt.edu/technology/support. Technical support is offered
24/7 through Pitt Help Desk ([email protected] OR 412-624-HELP(4357).
E-mail
The University provides all students with an e-mail account. Students should use their Pitt
account as their official e-mail address while at the University.
• SHRS faculty and staff will ONLY use the Pitt.edu address for electronic correspondence
• Pitt e-mail accounts can be easily accessed from the SHRS computer lab and e-mail
stations as well as any University CIS computing lab or email station
• Pitt e-mail can be accessed using the http://my.pitt.edu
• Pitt e-mail may be forwarded to another account (such as Gmail). To forward your
account go to http://accounts.pitt.edu
• Note: other e-mail accounts might not be able to handle some file attachments, e.g. files
you may need for class assignments. Your Pitt e-mail account will.
• Students must check Pitt e-mail account regularly or forward it to personal account
• For other Pitt account information and maintenance tools go to:
http://accounts.pitt.edu
• For more information or help with your e-mail account, contact SHRS IT Support at
60
Anthony & Filomena Pascasio Learning Resource Center (LRC)
4011 Forbes Tower
Hours: Monday through Friday 7:30am to 5:00pm
The LRC provides
▪ 12 additional student computers (see hardware and software listing above)
▪ 2 scanners
▪ Quiet study area
▪ University Printing Service Pickup
▪ Accessible computer station for students with disabilities
▪ USB/Mobile device charging stations
Health Sciences Library System
www.hsls.pitt.edu
412-648-8866
The Health Sciences Library System (HSLS) at the University of Pittsburgh comprises several libraries
that support the educational, research, patient care, and service activities to the schools of the health
sciences (Medicine, Dental Medicine, Pharmacy, Health and Rehabilitation Sciences, Nursing, and
Public Health), as well as the hospitals of the UPMC. The HSLS includes Falk Library of the Health
Sciences (home of the HSLS), the Libraries at UPMC Shadyside, and the Children’s Hospital of Pittsburgh
Libraries. HSLS Online (www.hsls.pitt.edu) is the gateway to extensive electronic resources for clinical
and research needs.

61
Parking/Transportation
http://www.pts.pitt.edu/parking/studentpermits.html
(412-383-7555)
Hourly/Daily Parking
If you are on the main Pitt campus regularly, you can find hourly and daily rates at the University's OC,
OH, PH, SN, and SO lots.
Short-term metered parking is available at more than 115 meters in the BQ, LC, PS, RA, SN, SR, and SQ
lots.
The Oakland neighborhood is also home to several private and city-owned parking facilities. Use this
list to guide you.
There is a garage located on Technology Drive across from BSP II building. You may park there on a
daily basis, or request a lease. Information will be provided to interested students by the Student
Services Administrator.
Public Transportation
All University of Pittsburgh Students, faculty, and staff may ride all Port Authority buses, trolleys, and
inclines within Allegheny County. Show the driver your current Panther I.D. Card to ride fare free.
Family members and guests must pay the full fare.
Shuttles are available for transport between main campus and BSP. These usually operate Monday-
Friday from 7 a.m. to 7 p.m. For the shuttle schedule see:
http://www.pittshuttle.com/
62
Disability Resources & Services
412-648-7890
The University has comprehensive resources available to the DPT students who have disabilities
through its Disability Resources and Services (DRS). DRS provides equal opportunities and support
services for academically qualified students with disabilities to ensure they are integrated as fully as
possible into the University experience. Their services include providing assistive technology,
specialized exam accommodations, interpreters and real-time captioning, assistance with
transportation and specialized housing accommodations. DRS is located on the first floor of the William
Pitt Union and can be contacted at 412-648-7890. With respect to DPT students:
Students with disabilities who require special testing, accommodations, or other classroom
modifications should notify, no later than the 2nd week of the term, their:
o
Vice-Chair
o
Course instructor(s)
o
Disability Resources and Services (DRS)
Students will be asked to provide documentation of their disability and any necessary
accommodations as prescribed by DRS.
Veteran Services
Veterans and dependents of disabled or deceased veterans may be eligible for benefits according to
federal administration guidelines. The University has an Office of Veterans Services located in Posvar
Hall. For additional information on Veterans Education Benefits, visit www.gibill.va.gov.
Student Health Services
http://www.studentaffairs.pitt.edu/shshome
Students in the University of Pittsburgh’s DPT program are prohibited from consulting or asking for
medical advice from principal faculty, adjunct faculty, guest lecturers, or any person in that capacity.
All students should seek out care from the Student Health Service (SHS) on the main campus, or their
local provider. The SHS is a primary care facility that features a health care clinic and pharmacy staffed
by medical doctors, nurses, nurse practitioners, a pharmacist, and other health care professionals.
Each student pays a student health fee each semester that gives them access to SHS, which also
provides a comprehensive array of educational programs and preventative medicine, including
women’s health services. SHS is located in the Wellness Center in Nordenberg Hall at 119 University
Place and the number is 412-383-1800. In an emergency, please call Pitt Police at 412-624-2121.
On-site services include
Dermatology
Lab Work
General Medicine
Nutrition Counseling
Gynecology
•
Orthopedics
•
Health Education Programs
•
Pharmacy
63
The Student Health Service is committed to:
•
Health Care: servicing the health needs of the University of Pittsburgh students.
•
Professionalism: Providing a professional and knowledgeable staff that is eager to help you in
the event of an illness or other health related concern.
•
Maintaining Confidentiality: Medical records are not released without the patient’s permission.
•
Advocating a Healthy Lifestyle: This philosophy will help to prevent many problems while
allowing you to lead a fuller, richer and longer life.
•
Providing Health Promoting Educational Aids: Counseling, literature, videotapes, films, courses,
seminars, and workshops.
General Medical Services covered by the Student Health Fee include
•
General Medicine
•
Contraceptive Options
•
Allergy Injections
•
Routine Lab Work
Specialty Medical Services covered by the Student Health Fee include
•
Dermatology
•
Gynecology
•
Internal Medicine
•
Orthopedics
University Counseling Center
http://www.studentaffairs.pitt.edu/cchome
The University Counseling Center provides comprehensive and confidential personal and academic
counseling to Pitt students free of charge. Staffed by psychologists, counselors, social workers,
psychiatrists, and pre-doctoral interns, the counseling center provides personal and group counseling
for a variety of conditions including ADHD/ADD, depression, drug and alcohol support, anxiety, grief,
sexual abuse, and more. The counseling center has day and evening hours by appointment and is
located in the Wellness Center in Nordenberg Hall. Please call 412-648-7930 for more information.
Comprehensive counseling and health services are available to students through the Student Health
Center and the Counseling Center, both of which are conveniently located on the main campus.
Counseling Center
https://www.studentaffai
rs.pitt.edu/cc/
Nordenberg Hall
412-648-7930
Sexual Assault Services
https://www.studentaffai
rs.pitt.edu/share/
Nordenberg Hall
412-648-7856
Student Health Service
Nordenberg Hall
412-383-1800
64
If You Have Not Paid the Student Health Fee
No problem! Student Health Services provide medical services to all University of Pittsburgh students,
regardless of Health Fee status.
We only ask that the students be prepared to meet the following conditions:
•
Monetary payment is accepted for all services provided by the Student Health Service.
•
MasterCard, Visa, Discover, personal Checks, and cash are acceptable forms of payment.
All charges for services provided must be paid for at the time of the visit.
*Remember, the Health Fee can be purchased at the Student Health Service upon request.
Reasons to Purchase
The Health Fee is primarily a once-per-term charge to the student. Its protection range spans the
length of the school term for which it was purchased, from the official first day of classes to the official
last day of classes.
The Fee was designed to provide students with virtually unlimited access to the majority of medical
services available at the Student Health Service facility at little or no additional cost.
At today’s health care prices, you won’t find a better bargain.
The once-per-term charge is not applicable to the Summer Term unless you take enough credits to be
classified as a full-time student.
How to Purchase
The Student Health Fee is mandatory for all full-time:
•
Undergraduate Students
•
Graduate Students
•
Professional Students
The Health Fee will appear as a line item on your tuition invoice. Part-time students may elect to pay
the Fee before the end of the add/drop period. Payment can be made at the Cashier’s Office,
Thackeray Hall, or at the Student Health Service Main Reception Desk.
The Health Fee enables the Student Health Service to provide health promotion programs, education,
and primary health care.

65
Coverage Limits
Payments for the following are not covered by the Student Services Health Fee:
•
Physical Examinations: Physical Examinations are given for a separate established cost.
•
Lab work, x-rays or immunizations associated with the physical examination.
•
Pharmacy: Prescriptions filled by a registered pharmacist, and over-the-counter drugs are also
available. While there is a charge for all items, prices are often lower than those in a
commercial drug store. Many third-party payers are accepted.
•
Referrals: The Student Health Service provides referrals to all medical specialties through
UPMC.
•
Payment for any services provided by any and all outsource facilities
•
Payment for treatment/services received somewhere else.
Optional Health Insurance Policies/Plans
•
The Student Health Service is designed as your source of primary health care during your
student years. There may, however, be a time when more extensive medical treatment or
emergency care is needed which is beyond our scope. Optional, third-party health insurance
policies are available to all students to provide additional major medical benefits for these
situations. These optional policies cover the medical services administered by other medical
facilities only, and do not cover services provided by the Student Health Service.
UPMC Health Plan for Students
The University has joined with UPMC Health Plan, the insurance division of the world-class University
of Pittsburgh Medical Center (UPMC) to offer comprehensive/affordable student health insurance.
•
Health Plans and premium rates are available for a single student.
•
Insurance may also be purchased for the spouse and children of a student; please call number
listed below for additional information.
We encourage you to consider UPMC Health Plan student health insurance as a means of protecting
yourself against unexpected, unforeseen medical expenses that could temporarily or permanently
interrupt your graduate career.
For more information on how UPMC Health Plan’s student insurance and health promotion programs
can maintain you and/or your dependents current and future health, please call 1-877-381-3764 to
speak with a program representative.

66
Liability Insurance
• Students enrolled in Clinical Education must carry professional liability insurance. This is
arranged through the University and the cost is reflected on the fall term tuition bill each year.
• The insurance cycles run from August 1-July 31 each year.
• Verification certificates are provided to the clinical sites upon request.
67
Student Resources
University: www.pitt.edu
SHRS: www.shrs.pitt.edu/
DPT Program: www.shrs.pitt.edu/DPT/
Academic Calendar: http://www.provost.pitt.edu/information-on/calendar.html
Academic Integrity: https://www.shrs.pitt.edu/academicpolicies/
http://www.provost.pitt.edu/info/ai1.html
CAPTE: www.capteonline.org
Career Center: http://www.studentaffairs.pitt.edu/cdpa
Disability Resources: http://www.studentaffairs.pitt.edu/drs/
Diversity & Inclusion http://www.studentaffairs.pitt.edu/dean/diversity/
DPT Admissions: https://www.shrs.pitt.edu/dpt/admission
DPT Student Outcomes: https://www.shrs.pitt.edu/DPTStudentOutcomes/
DPT Students’ Webpage: http://pittphysicaltherapy.com/
DPT Technical Standards: https://www.shrs.pitt.edu/admissions_DPT/
Exploring Pittsburgh http://www.visitpittsburgh.com/
http://www.coolpgh.pitt.edu/
Financial Aid: https://oafa.pitt.edu/financialaid/applying-for-aid/graduate-school-instructions/
Grading: http://catalog.upp.pitt.edu/content.php?catoid=6&navoid=47#grading-
policy-and-records
Graduate & Professional http://www.gpsa.pitt.edu/
Student Government
Graduate and Professional
Studies Catalog: https://catalog.upp.pitt.edu/index.php
Health and Wellness: https://www.studentaffairs.pitt.edu/shs/
69
Library Links:
Hillman: http://www.library.pitt.edu/hillman
Health Science: http://www.hsls.pitt.edu
University of Pittsburgh: http://www.pitt.edu/libraries.html
Off-campus living in Pittsburgh: http://www.ocl.pitt.edu/
Office of the Registrar
(University of Pittsburgh): http://www.registrar.pitt.edu/
Office of Veteran Services: http://www.veterans.pitt.edu/
Pandemic Resources
University of Pittsburgh: https://www.coronavirus.pitt.edu/
SHRS: https://www.shrs.pitt.edu/covid-19
CDC: https://www.cdc.gov/coronavirus/2019-ncov/index.html
Placement and Career Services: http://www.careers.pitt.edu/
Policy and Procedures: http://www.shrs.pitt.edu/current-students/academic-policies
General: http://www.pitt.edu/~graduate/policies.html
Grading: http://www.registrar.pitt.edu/grades.html
HIPAA: http://www.ehs.pitt.edu/
Safety: http://www.ehs.pitt.edu/
SHRS new student orientation: https://www.shrs.pitt.edu/orientation/
SHRS Student Resources: https://www.shrs.pitt.edu/StudentResources/
Title IX: http://www.titleix.pitt.edu/
Travel Grant Opportunities: http://www.shrs.pitt.edu/student.aspx?id=291
Tuition/Financial Aid at Pitt: https://ir.pitt.edu/graduate-tuition/
http://www.oafa.pitt.edu/fahome.aspx

70
SHRS Contacts
SHRS Resource Contacts
(see SHRS Directory at www.shrs.pitt.edu for Departmental and other listings.)
Admissions
Jessica Maguire, Director 412-383-6557
4021 Forbes Tower
Joni Keating, Admissions Administrator 412-383- 6558
4020 Forbes Tower
Dean’s Office
Jen Falo, Assistant to the Dean 412-383-6560
4028 Forbes Tower
Information Services (IS) Support Desk 412-383-6657
6048 Forbes Tower
Lost and Found – Forbes Tower 412-383-6554
4024 Forbes Tower
Registrar and Student Services
Kellie Beach, Registrar, Director and Ombudsman 412-383-6554
4024 Forbes Tower
Jordan Ulrich, Student Services Coordinator 412-383-6551
4024 Forbes Tower

71
Department of Physical Therapy Contacts
PT Office Telephone: 412-383-6630 Fax: 412-648-5970
Name
Telephone
E-mail Address
Christopher Bise, MS, DPT, OCS
412-383-5250
Allyn Bove, PT, DPT
412-624-9255
ams453@pitt.edu
Jennifer Brach, PhD, PT
412-383-6533
jbrach@pitt.edu
George Carvell, PhD, PT
412-383-6639
Wei-Neng Chuang, MS, PT
412-383-6635
wec12@pitt.edu
Ronna Delitto, MHS, PT
412-383-6635
Jean Evans, Administrator
412-383 -9865
G. Kelley Fitzgerald, PhD, PT, FAPTA
412-383-6643
Lynn Fitzgerald, MEd, DPT
412-383-6638
Janet Freburger, PT, PhD
Rick Joreitz, PT, DPT
412-383-3281
412-648-8210
rej13@pitt.edu
Brooke Klatt, PT, PhD
412-6482215
bnk12@pitt.edu
Lauren Lagana, Administrator
412-383-2184
Alexandra Gil PhD, PT
412-383-6714
Corinne Grubb, Administrator
412-383-8169
Karthik Hariharan, MS, PT
412-383-6645
Tara Ridge Hankin, MS, PT
Andrea Hergenroeder, PhD, PT, CCS
Vicki Hornyak, DPT, GCS
412-383-4619
412-383-6964
412-624-1026
James J. Irrgang, PhD, PT, FAPTA, ATC
412-383-9865
jirrgan[email protected]
Deborah Josbeno, PhD, PT, NCS, CSCS
412-383-6713
Samannaaz Khoja, PhD, PT
412-383-6868
M. Kathleen Kelly, PhD, PT
412-383-6637
Caryn Loehr, Administrator
412-624-6292
Sara Piva, PhD, PT
Adam Popchak, PhD, PT
412-383-6712
412-3836627
Michael Schneider, PhD, DC
412-383-6640
Patrick Sparto, PhD, PT
412-383-6729
Andrew Sprague, PhD, PT
412-383-6632
Joel Stevans, PhD, DC
412-383-6652
Jms36[email protected]
Mike Timko, PT, MS, FAAOMPT
412-383-6578
mtimko@pitt.edu
Debra Utterback, Administrator
412-383-6942
Jessie VanSwearingen, PhD, PT, FAPTA
412-383-6634
David Wert, PhD, PT
412-383-5397
Susan Whitney, PhD, PT, FAPTA, ATC, NCS
412-383-6642
Terri Wubben, PT, MPM
412-383-6732
72
A. Institution
Policies
Student-Related Policies and Procedures
University of Pittsburgh Graduate and Professional Bulletin:
Table of Contents:
http://catalog.upp.pitt.edu/content.php?catoid=6&navoid=4
7 Academic Integrity: http://www.shrs.pitt.edu/current-students/academic-policies
Accreditation: http://ir.pitt.edu/factbook/fbweb99/general/Accred99.htm
Applying: http://catalog.upp.pitt.edu/content.php?catoid=6&navoid=47#admission
Financial aid: http://catalog.upp.pitt.edu/content.php?catoid=6&navoid=47#financial
Student rights and responsibilities: http://www.shrs.pitt.edu/current-students/student-handbooks
Student Code of Conduct: http://www.studentaffairs.pitt.edu/wp-
content/uploads/2016/11/2016_Code_of_Conduct_Nov4.pdf
University of Pittsburgh Office of Admissions & Financial
Aid: http://oafa.pitt.edu/learn-about-aid/
https://ir.pitt.edu/graduate-tuition/
University of Pittsburgh Judicial Process: http://www.studentaffairs.pitt.edu/conduct/process/
Provost Guidance related to students: http://www.provost.pitt.edu/information-
on/guidelines.html Anti-Harassment and Nondiscrimination
Anti-Harassment Policy Statement: https://provost.pitt.edu/information-
on/antiharassment_statement Nondiscrimination, Equal Opportunity, and Affirmative Action
Recognizing Religious Observances:
https://provost.pitt.edu/recognizing-religious-
observances University Sexual Harassment Policy:
http://www.titleix.pitt.edu/policies-procedures
Privacy and Confidentiality Rights
Confidentiality of Medical Information
Gramm-Leach-Bliley Act: Safeguarding Customer Information
B. SHRS Policies
Academic Integrity: https://shrs.pitt.edu/academicpolicies/
Admissions:
https://www.shrs.pitt.edu/Admissions.aspx?id=348
8 Financial Information: https://www.shrs.pitt.edu/financialinformation/
University of Pittsburgh, SHRS Graduate Student Handbook:
Graduate Student Handbook:
https://shrs.pitt.edu/SHRShandbooks
/ Index: Pages 1, 2
Policies and procedures: Page 6
Nondiscrimination: Page 6
Grading: Page 10
Financial Aid: Page 23 https://oafa.pitt.edu/financialaid/applying-for-aid/graduate-school-instructions/
Scholarships: Page 23 https://www.shrs.pitt.edu/scholarships/
74
C. Program Policies
DPT Program Website: https://www.shrs.pitt.edu/DPT/
Introduction: https://www.shrs.pitt.edu/PT/
Accreditation: http://www.capteonline.org/home.aspx
Clinical Partners: https://www.shrs.pitt.edu/dpt/clinical-partners
Complaint Registration: http://www.capteonline.org/Complaints/
Curriculum: https://www.shrs.pitt.edu/dpt/curriculum
DPT Education Experiences: https://www.shrs.pitt.edu/dpt/curriculum/education-experiences
DPT Program Facts: https://www.shrs.pitt.edu/DPT_FAQ/
Grading: http://www.registrar.pitt.edu/grades.html
Outcome Information: https://www.shrs.pitt.edu/DPTStudentOutcomes/

75
Main Campus Map
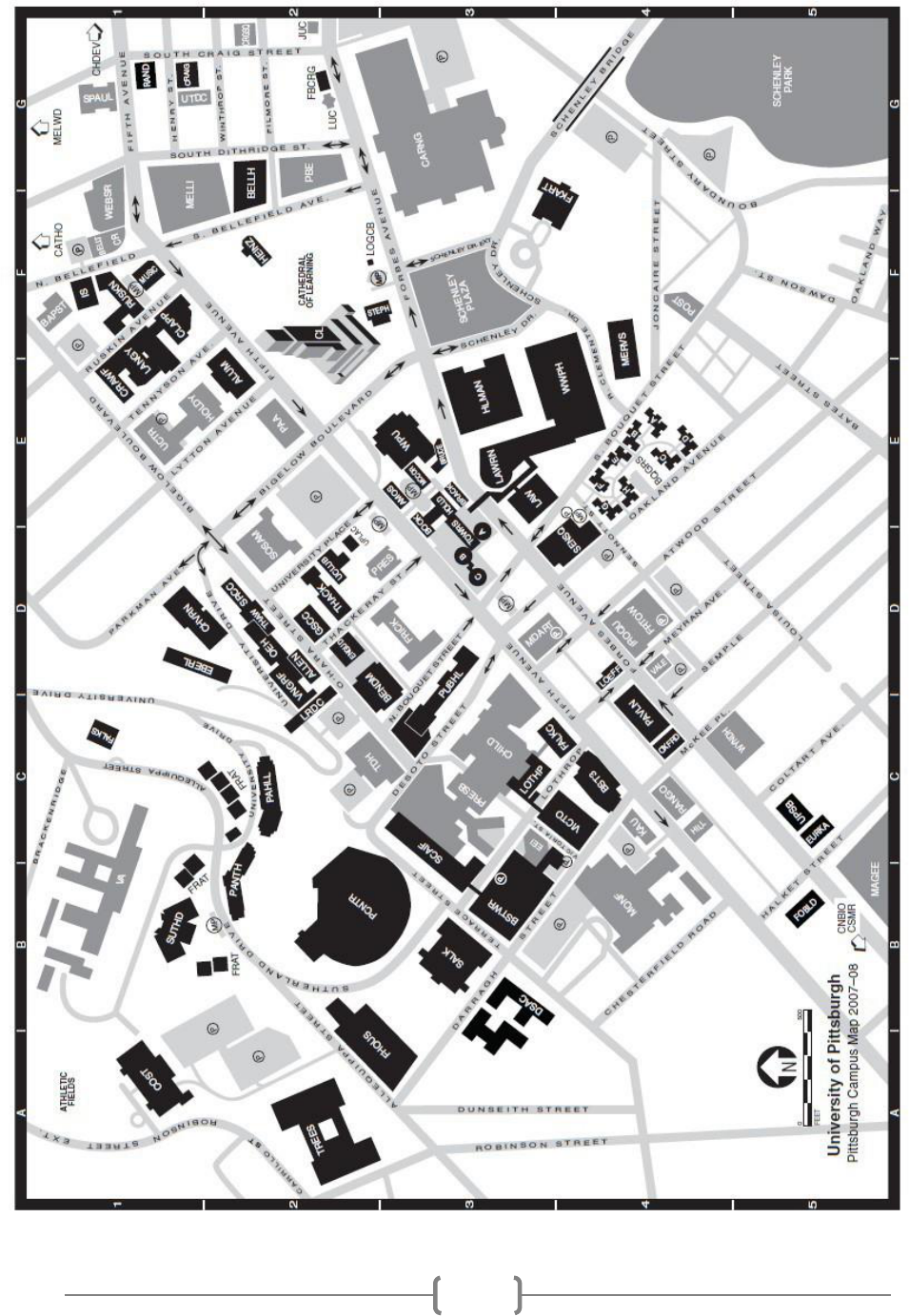
76

77
78
APPENDICES

79
Technical Standards Required for the DPT Program
To acquire requisite knowledge and skills to practice as a physical therapist, graduate students
must be able to function in a broad variety of clinical situations and provide a wide spectrum of
patient care. Students must possess certain skills and abilities to successfully complete both the
didactic and clinical components of the curriculum with or without reasonable accommodations,
regardless of disability status. All graduates must be able to perform tasks such as: taking a case
history, performing examination tests and measures, completing an evaluation, and performing
manual interventions. They must also be able to synthesize these findings into a physical therapy
diagnosis and plan of treatment.
These skills and abilities are divided into five areas: communication, motor, intellectual-
cognitive, sensory-observational and behavioral-social.
Students must be able to undertake all academic (clinical and
didactic requirements) to the satisfaction of faculty to become competent and reliable practitioners.
To this end, the Faculty of the Department of Physical Therapy has established
criteria (Technical Standards) that students must possess in order to enroll in, and to continue
in academic courses and clinical placements required for the DPT degree.
General Guidelines
The Doctor of Physical Therapy (DPT) degree is typically a three-year program
that requires the acquisition of professional attitudes, skills and behavior as well as the
accumulation of scientific knowledge. The DPT degree certifies that the student has acquired the
broad base of knowledge and skills required for the practice of physical therapy and is eligible to
take the professional licensing examination. These standards are rigorous and exacting
so admission can be offered only to those individuals best-
qualified to meet the performance standards of the profession.
Acceptance to the DPT program is offered to those who present the highest qualifications f
or the study and practice of physical therapy. Graduates of the program must have the knowledge
and skills to function in a variety of clinical situations and to render a wide spectrum of patient car
e.
Candidates for the DPT degree must have somatic sensation and the functional use of the
necessary senses. Skills will be lessened if the student does not have functional use of the sense of
balance and sufficient motor function to permit them to carry out the activities described in the
sections that follow. They must be able to consistently, quickly and accurately integrate
all information received by
whatever sense(s) are employed, and they must have the intellectual ability to learn,
integrate, analyze and synthesize data.

80
Candidates for the DPT degree must have abilities and skills in the five areas outlined below.
Communication. A student must possess adequate communication skills to:
o Communicate effectively and proficiently in oral and written English
English language skills must be at a level that can be easily understood by clients and colleagues
for general interactions, for administration of tests and implementation of treatment as judged by a
panel of PT faculty.
• Read and write to meet didactic and clinical demands
• Demonstrate and perceive non-verbal communication with patients that is appropriate for culture
and context
• Communicate with patients, families, peers and colleagues at an appropriate and professional level
• Clearly record examination results, treatment observations and treatment plans in a
reasonable amount of time
• Accurately convey information with relevance and cultural sensitivity
• Effectively receive and send verbal communication in emergency situations
• Recognize and promptly respond to the patient’s emotional communications such as
sadness, worry, agitation, pain and lack of comprehension of therapist communication
Motor. A student must possess adequate motor skills to:
• Sustain the necessary physical activity level required in classroom and clinical activities
• Respond quickly in the event of an emergency situation to provide patients a safe environment
• Access transportation to clinical and didactic placement sites
• Prepare the clinical environment without compromising best practice guidelines
• Assume and maintain a variety of body postures (e.g. sitting, standing, walking, bending, squatting,
kneeling, stair climbing, reaching forward, reaching overhead, turning and movement of the trunk and
neck in all directions) so as to sufficiently perform patient examination and intervention procedures
• Demonstrate appropriate psychomotor skills for performing tests and measures for
patient examination
• Execute appropriate psychomotor movements required for manual handling and manipulation
of various object/person sizes and weights including lifting and transferring patients, guarding patients
during gait training on level surfaces/uneven surfaces/ramps/stairs, pushing and pulling to provide
resistance and to assist in maneuvering patients. Students may be required to:
o Safely lift up to 50 lbs independently
o Safely lift up to 200 lbs with assistance
o Safely push and pull up to 200 lbs
• Balance self and provide support and balance to patients on a variety of surfaces including level and
uneven ground, ramps, curbs, and stairs
• Have sufficient endurance to effectively manage patient care
• Access technology for clinical and didactic requirements
• Complete an episode of care within a reasonable time frame to effectively manage the patient
Sensory/Observational. A student must possess adequate sensory skills to:
• Effectively observe and function (in visual and auditory modalities) in both clinical and
didactic settings
• Record and evaluate physical status as well as verbal and non-verbal responses to sensory stimuli
• Visually assess treatment equipment, goniometric measures, normal/abnormal color changes and
integrity of the skin, pupillary changes, postures, and normal/abnormal movement patterns
81
• Perform effective auscultation/auditory evaluation inclusive of but not limited to: lungs,
heart, apical pulse, blood pressure, joint noises, prostheses
• Listen for environmental cues inclusive of but not limited to: phones, overhead paging systems, alar
ms, verbal communication in a setting with competing ambient noise
• Provide appropriate tactile feedback related to safe application of gradient pressures during
examination and intervention (including but not limited to: palpation, manual muscle testing, joint
mobility, percussion, massage)
Intellectual/Cognitive. A student must possess adequate intellectual and cognitive skills to:
• Comprehend, retain, assimilate, analyze, synthesize, integrate concepts and problem solve
• Formulate written and verbal assessments and therapeutic judgments to meet didactic
and clinical demands in a reasonable time frame
• Identify and communicate the limits of their own knowledge and skills
• Utilize resources to increase their own base of knowledge and skills
• Comprehend three-dimensional relationships, the spatial and functional relationships of
structures, and analyze and apply this information for problem solving and decision-making.
• Comprehend text, numbers and graphs
• Gather, appraise, and evaluate patient information collected during history, examinations, and
throughout patient/client management to formulate hypotheses and make clinical decisions (diagnoses,
prognoses, and plans of care).
Behavioral/Social. A student must possess:
• Appropriate interpersonal skills and the demeanor and rapport necessary for quality patient care
• The capacity to maintain composure and continue to function well during periods of high stress
• The perseverance, diligence and commitment to complete professional program requirements
• The flexibility and the ability to adjust to the changing situations and uncertainty inherent in clinical
situations
• The ability to critically evaluate his or her own performance and identify tactics to improve perform
ance, both with and independent of faculty assistance
• Compassion, integrity and empathy for others
• The ability to reason morally and practice physical therapy in an ethical manner
• The ability to demonstrate appropriate assertiveness, delegate responsibilities, and function as part
of a physical therapy team
• The ability to show respect for individuals with disabilities and those of differing cultural and
linguistic backgrounds, races, religions and/or sexual orientations
Candidates for graduate degrees in the Department of Physical Therapy are required to meet the above
technical standards, with or without reasonable accommodation, regardless of disability. Disability self- identification is
voluntary and confidential. The University of Pittsburgh offers reasonable accommodation for qualified, eligible
students with disabilities. Please contact our Disability Resources and Services (412-648-7890)
for information regarding documentation guidelines.
82
University of Pittsburgh
Bridgeside Point 1
100 Technology Drive-Suite 210
Pittsburgh, PA 15219-3130
412-383-6630
Fax: 412-648-5970
www.shrs.pitt.edu/PT
School of Health and Rehabilitation
Sciences Department of Physical
Therapy
Technical Standards Statement
ALL STUDENTS ADMITTED TO THE DPT PROGRAM
MUST SIGN THE STATEMENT BELOW
and submit it to the Department office at
210 Bridgeside Point 1
I certify that I have read and understand the attached echnical standards and I believe to
the best of my knowledge that I am able to meet each of these standards
□without accommodation
□with reasonable accommodation for a disability
I understand that if I am unable to meet these standards with or without reasonable
accommodation now or in the future, I will be denied permission to enroll or continue in
the program.
Please Print Name
Signature Date
83
APPENDICES
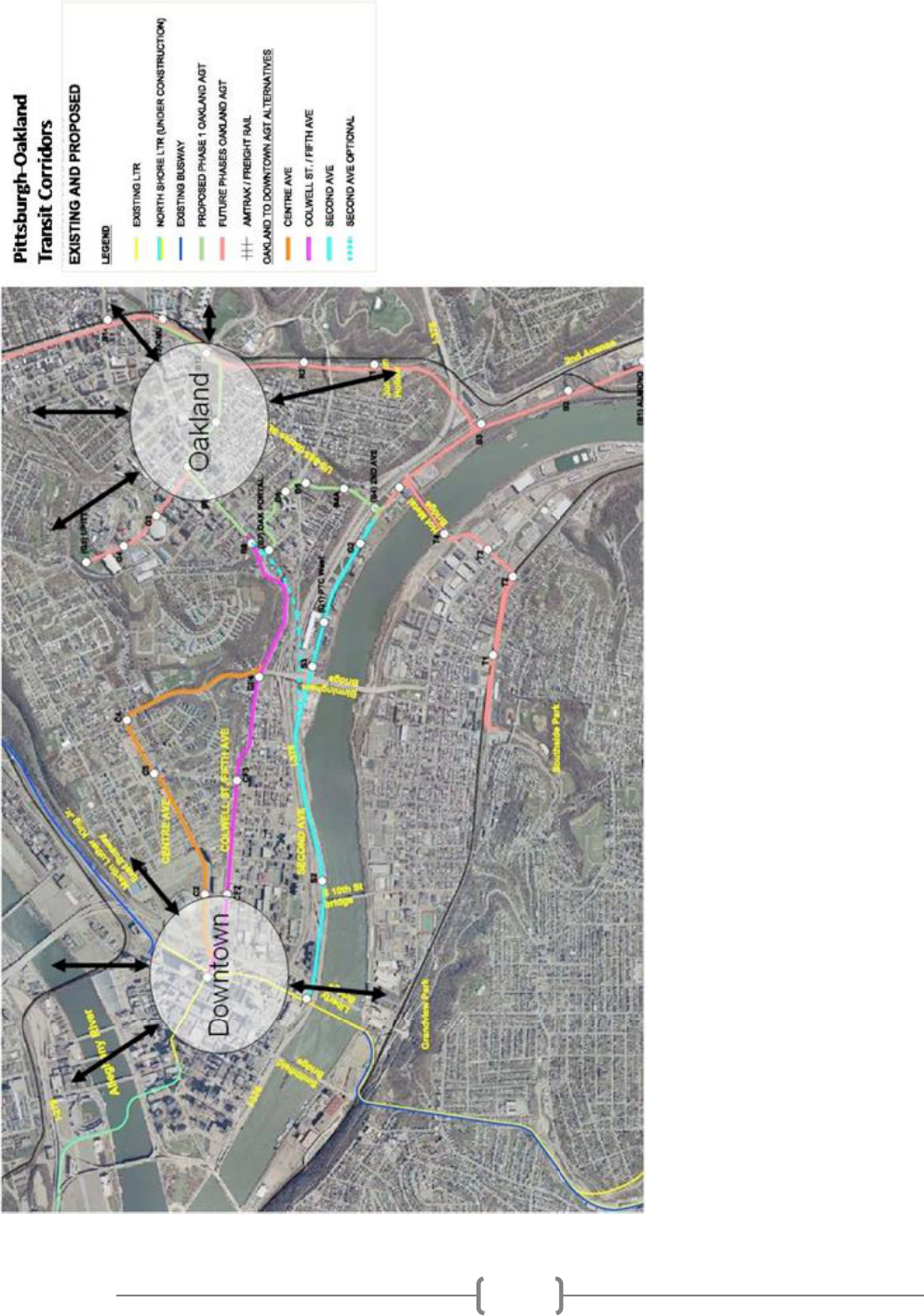
84

85

86
APPENDICES

87
Technical Standards Required for the DPT Program
To acquire requisite knowledge and skills to practice as a physical therapist, graduate students
must be able to function in a broad variety of clinical situations and provide a wide spectrum of
patient care. Students must possess certain skills and abilities to successfully complete both the
didactic and clinical components of the curriculum with or without reasonable accommodations,
regardless of disability status. All graduates must be able to perform tasks such as: taking a case
history, performing examination tests and measures, completing an evaluation, and performing
manual interventions. They must also be able to synthesize these findings into a physical therapy
diagnosis and plan of treatment.
These skills and abilities are divided into five areas: communication, motor, intellectual-
cognitive, sensory-observational and behavioral-social. Students must be able to undertake all
academic (clinical and didactic requirements) to the satisfaction of faculty to become competent and
reliable practitioners. To this end, the Faculty of the Department of Physical Therapy has established
criteria (Technical Standards) that students must possess in order to enroll in, and to continue in
academic courses and clinical placements required for the DPT degree.
General Guidelines
The Doctor of Physical Therapy (DPT) degree is typically a three-year program that requires
the acquisition of professional attitudes, skills and behavior as well as the accumulation of scientific
knowledge. The DPT degree certifies that the student has acquired the broad base of knowledge and
skills required for the practice of physical therapy and is eligible to take the professional licensing
examination. These standards are rigorous and exacting so admission can be offered only to those
individuals best-qualified to meet the performance standards of the profession.
Acceptance to the DPT program is offered to those who present the highest qualifications for
the study and practice of physical therapy. Graduates of the program must have the knowledge and
skills to function in a variety of clinical situations and to render a wide spectrum of patient care.
Candidates for the DPT degree must have somatic sensation and the functional use of the necessary
senses. Skills will be lessened if the student does not have functional use of the sense of balance and
sufficient motor function to permit them to carry out the activities described in the sections that
follow. They must be able to consistently, quickly and accurately integrate all information received by
whatever sense(s) are employed, and they must have the intellectual ability to learn, integrate, analyze
and synthesize data.

88
Candidates for the DPT degree must have abilities and skills in the five areas outlined below.
Communication. A student must possess adequate communication skills to:
•
Communicate effectively and proficiently in oral and written English
English language skills must be at a level that can be easily understood by clients and colleagues for
general interactions, for administration of tests and implementation of treatment as judged by a panel of
PT faculty.
•
Read and write to meet didactic and clinical demands
•
Demonstrate and perceive non-verbal communication with patients that is appropriate for
culture and context
•
Communicate with patients, families, peers and colleagues at an appropriate and
professional level
•
Clearly record examination results, treatment observations and treatment plans in a
reasonable amount of time
•
Accurately convey information with relevance and cultural sensitivity
•
Effectively receive and send verbal communication in emergency situations
•
Recognize and promptly respond to the patient’s emotional communications such as
sadness, worry, agitation, pain and lack of comprehension of therapist communication
Motor. A student must possess adequate motor skills to:
•
Sustain the necessary physical activity level required in classroom and clinical activities
•
Respond quickly in the event of an emergency situation to provide patients a safe environment
•
Access transportation to clinical and didactic placement sites
•
Prepare the clinical environment without compromising best practice guidelines
•
Assume and maintain a variety of body postures (e.g. sitting, standing, walking, bending,
squatting, kneeling, stair climbing, reaching forward, reaching overhead, turning and
movement of the trunk and neck in all directions) so as to sufficiently perform patient
examination and intervention procedures
•
Demonstrate appropriate psychomotor skills for performing tests and measures for
patient examination
•
Execute appropriate psychomotor movements required for manual handling and manipulation
of various object/person sizes and weights including lifting and transferring patients, guarding
patients during gait training on level surfaces/uneven surfaces/ramps/stairs, pushing and
pulling to provide resistance and to assist in maneuvering patients. Students may be required
to:
❖
Safely lift up to 50 lbs independently
❖
Safely lift up to 200 lbs with assistance
❖
Safely push and pull up to 200 lbs
•
Balance self and provide support and balance to patients on a variety of surfaces including level
and uneven ground, ramps, curbs, and stairs
•
Have sufficient endurance to effectively manage patient care
•
Access technology for clinical and didactic requirements
•
Complete an episode of care within a reasonable time frame to effectively manage the patient
89
Sensory/Observational. A student must possess adequate sensory skills to:
•
Effectively observe and function (in visual and auditory modalities) in both clinical and
didactic settings
•
Record and evaluate physical status as well as verbal and non-verbal responses to
sensory stimuli
•
Visually assess treatment equipment, goniometric measures, normal/abnormal color
changes and integrity of the skin, pupillary changes, postures, and normal/abnormal
movement patterns
•
Perform effective auscultation/auditory evaluation inclusive of but not limited to: lungs,
heart, apical pulse, blood pressure, joint noises, prostheses
•
Listen for environmental cues inclusive of but not limited to: phones, overhead paging
systems, alarms, verbal communication in a setting with competing ambient noise
• Provide appropriate tactile feedback related to safe application of gradient pressures
during examination and intervention (including but not limited to: palpation, manual
muscle testing, joint mobility, percussion, massage)
Intellectual/Cognitive. A student must possess adequate intellectual and cognitive skills to:
•
Comprehend, retain, assimilate, analyze, synthesize, integrate concepts and problem solve
•
Formulate written and verbal assessments and therapeutic judgments to meet didactic
and clinical demands in a reasonable time frame
•
Identify and communicate the limits of their own knowledge and skills
•
Utilize resources to increase their own base of knowledge and skills
•
Comprehend three-dimensional relationships, the spatial and functional relationships of
structures, and analyze and apply this information for problem solving and decision-making.
•
Comprehend text, numbers and graphs
•
Gather, appraise, and evaluate patient information collected during history, examinations, and
throughout patient/client management to formulate hypotheses and make clinical decisions
(diagnoses, prognoses, and plans of care).
Behavioral/Social. A student must possess:
•
Appropriate interpersonal skills and the demeanor and rapport necessary for quality patient care
•
The capacity to maintain composure and continue to function well during periods of high stress
•
The perseverance, diligence and commitment to complete professional program requirements
•
The flexibility and the ability to adjust to the changing situations and uncertainty inherent in
clinical situations
•
The ability to critically evaluate his or her own performance and identify tactics to improve
performance, both with and independent of faculty assistance
•
Compassion, integrity and empathy for others
•
The ability to reason morally and practice physical therapy in an ethical manner
•
The ability to demonstrate appropriate assertiveness, delegate responsibilities, and function
as part of a physical therapy team
•
The ability to show respect for individuals with disabilities and those of differing cultural and
linguistic backgrounds, races, religions and/or sexual orientations

90
Candidates for graduate degrees in the Department of Physical Therapy are required to meet the
above technical standards, with or without reasonable accommodation, regardless of disability.
Disability self- identification is voluntary and confidential. The University of Pittsburgh offers
reasonable accommodation for qualified, eligible students with disabilities. Please contact our
Disability Resources and Services (412-648-7890) for information regarding documentation guidelines.
91
University of Pittsburgh
Bridgeside Point 1
100 Technology Drive-Suite 210
Pittsburgh, PA 15219-3130
412-383-6630
Fax: 412-648-5970
www.shrs.pitt.edu/PT
School of Health and Rehabilitation Sciences
Department of Physical Therapy
Technical Standards Statement
ALL STUDENTS ADMITTED TO THE DPT PROGRAM
MUST SIGN THE STATEMENT BELOW
and submit it to the Department office at
210 Bridgeside Point 1
I certify that I have read and understand the attached technical standards and I believe to
the best of my knowledge that I am able to meet each of these standards
□ without accommodation
□ with reasonable accommodation for a disability
I understand that if I am unable to meet these standards with or without reasonable
accommodation now or in the future, I will be denied permission to enroll or continue in
the program.
Please Print Name
Signature Date

92

93